
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Drug/Regimen
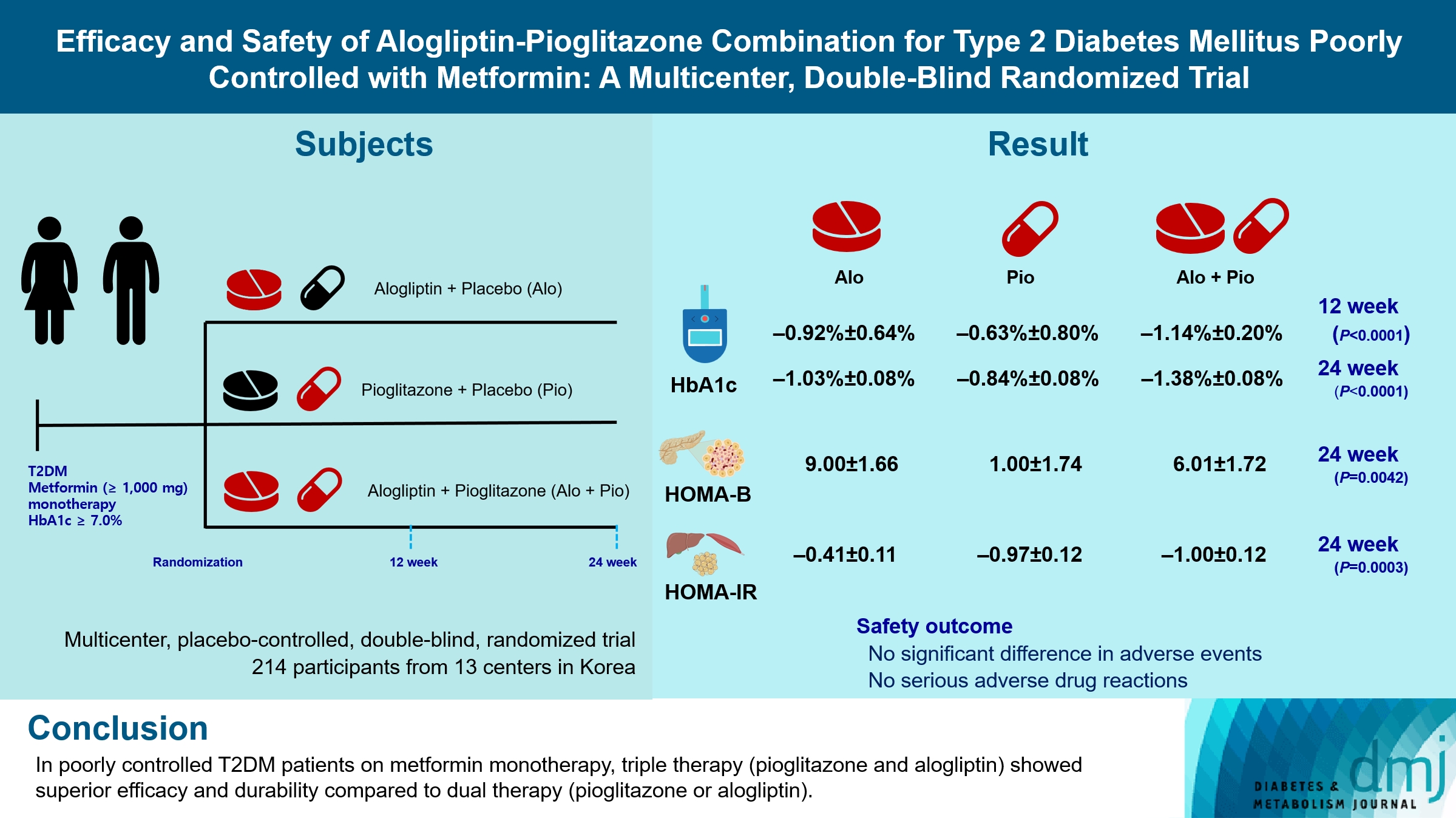
- Efficacy and Safety of Alogliptin-Pioglitazone Combination for Type 2 Diabetes Mellitus Poorly Controlled with Metformin: A Multicenter, Double-Blind Randomized Trial
- Ji-Yeon Park, Joonyub Lee, Yoon-Hee Choi, Kyung Wan Min, Kyung Ah Han, Kyu Jeung Ahn, Soo Lim, Young-Hyun Kim, Chul Woo Ahn, Kyung Mook Choi, Kun-Ho Yoon, the Practical Evidence of Antidiabetic Combination Therapy in Korea (PEAK) study investigators
- Received August 7, 2023 Accepted November 30, 2023 Published online April 23, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0259 [Epub ahead of print]
- 191 View
- 8 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Guidelines for switching to triple combination therapy directly after monotherapy failure are limited. This study investigated the efficacy, long-term sustainability, and safety of either mono or dual add-on therapy using alogliptin and pioglitazone for patients with type 2 diabetes mellitus (T2DM) who did not achieve their target glycemic range with metformin monotherapy.
Methods
The Practical Evidence of Antidiabetic Combination Therapy in Korea (PEAK) was a multicenter, placebo-controlled, double-blind, randomized trial. A total of 214 participants were randomized to receive alogliptin+pioglitazone (Alo+Pio group, n=70), alogliptin (Alo group, n=75), or pioglitazone (Pio group, n=69). The primary outcome was the difference in glycosylated hemoglobin (HbA1c) levels between the three groups at baseline to 24 weeks. For durability, the achievement of HbA1c levels <7% and <6.5% was compared in each group. The number of adverse events was investigated for safety.
Results
After 24 weeks of treatment, the change of HbA1c in the Alo+Pio, Alo, and Pio groups were –1.38%±0.08%, –1.03%±0.08%, and –0.84%±0.08%, respectively. The Alo+Pio group had significantly lower HbA1c levels than the other groups (P=0.0063, P<0.0001) and had a higher proportion of patients with target HbA1c achievement. In addition, insulin sensitivity and β-cell function, lipid profiles, and other metabolic indicators were also improved. There were no significant safety issues in patients treated with triple combination therapy.
Conclusion
Early combination triple therapy showed better efficacy and durability than the single add-on (dual) therapy. Therefore, combination therapy with metformin, alogliptin, and pioglitazone is a valuable early treatment option for T2DM poorly controlled with metformin monotherapy.
- Drug/Regimen
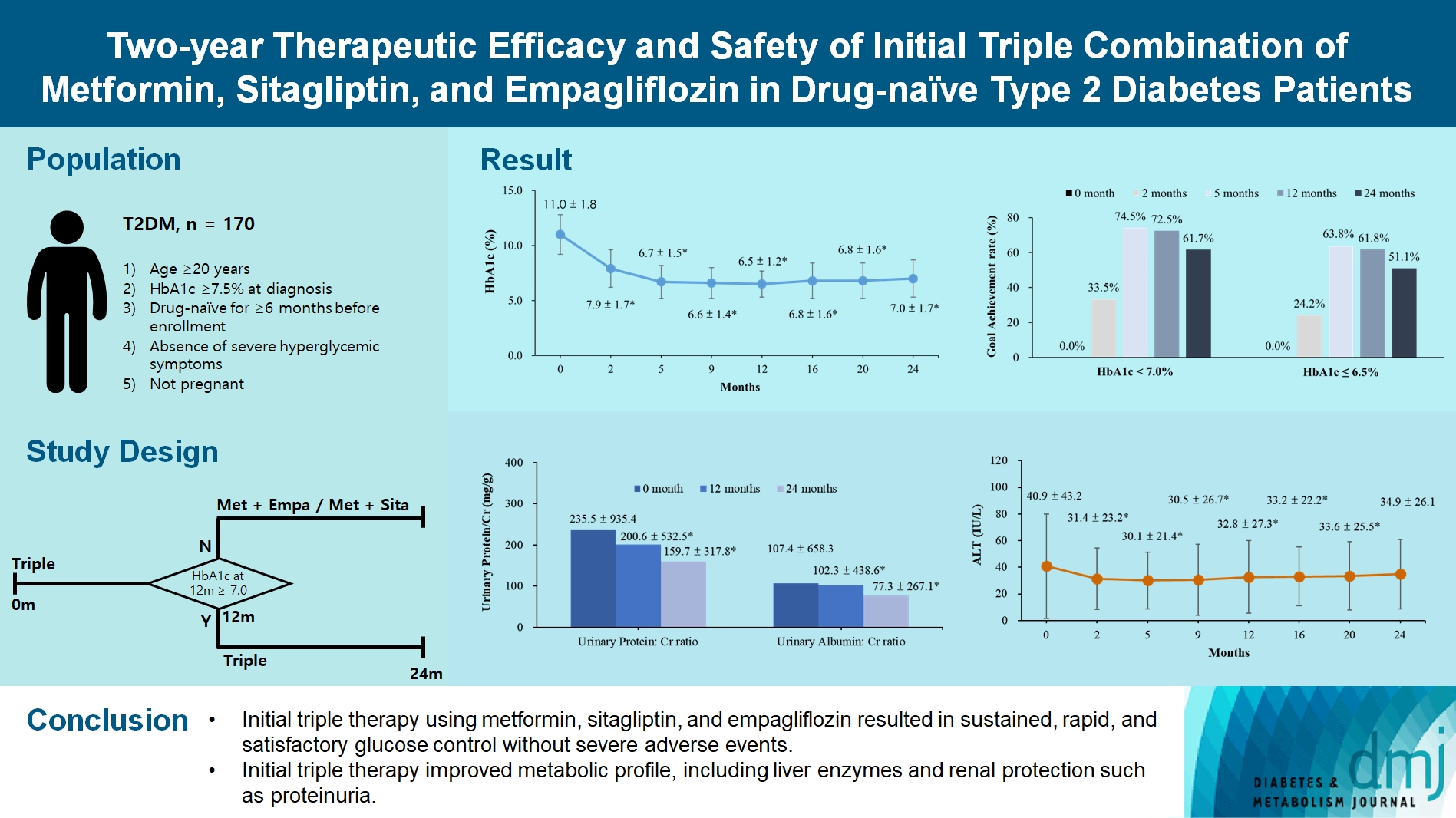
- Two-Year Therapeutic Efficacy and Safety of Initial Triple Combination of Metformin, Sitagliptin, and Empagliflozin in Drug-Naïve Type 2 Diabetes Mellitus Patients
- Young-Hwan Park, Minji Sohn, So Yeon Lee, Soo Lim
- Diabetes Metab J. 2024;48(2):253-264. Published online January 26, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0128
- 1,707 View
- 273 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We investigated the long-term efficacy and safety of initial triple therapy using metformin, a dipeptidyl peptidase-4 inhibitor, and a sodium-glucose cotransporter-2 inhibitor, in patients with type 2 diabetes mellitus.
Methods
We enrolled 170 drug-naïve patients with glycosylated hemoglobin (HbA1c) level >7.5% who had started triple therapy (metformin, sitagliptin, and empagliflozin). Glycemic, metabolic, and urinary parameters were measured for 24 months.
Results
After 24 months, HbA1c level decreased significantly from 11.0%±1.8% to 7.0%±1.7%. At 12 and 24 months, the rates of achievement of the glycemic target goal (HbA1c <7.0%) were 72.5% and 61.7%, respectively, and homeostasis model assessment of β-cell function and insulin resistance indices improved. Whole-body fat percentage decreased by 1.08%, and whole-body muscle percentage increased by 0.97% after 24 months. Fatty liver indices and albuminuria improved significantly. The concentration of ketone bodies was elevated at the baseline but decreased after 24 months. There were no serious adverse events, including ketoacidosis.
Conclusion
Initial triple combination therapy with metformin, sitagliptin, and empagliflozin led to achievement of the glycemic target goal, which was maintained for 24 months without severe hypoglycemia but with improved metabolic function and albuminuria. This combination therapy may be a good strategy for drug-naïve patients with type 2 diabetes mellitus.
- Others
- Glucose Regulation after Partial Pancreatectomy: A Comparison of Pancreaticoduodenectomy and Distal Pancreatectomy in the Short and Long Term
- Jun Suh Lee, Minji Sohn, Kyuho Kim, Yoo-Seok Yoon, Soo Lim
- Diabetes Metab J. 2023;47(5):703-714. Published online June 22, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0205

- 1,639 View
- 150 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Long term quality of life is becoming increasingly crucial as survival following partial pancreatectomy rises. The purpose of this study was to investigate the difference in glucose dysregulation after pancreaticoduodenectomy (PD) or distal pancreatectomy (DP).
Methods
In this prospective observational study from 2015 to 2018, 224 patients who underwent partial pancreatectomy were selected: 152 (67.9%) received PD and 72 (32.1%) received DP. Comprehensive assessment for glucose regulation, including a 75 g oral glucose tolerance test was conducted preoperatively, and 1, 12, and 52 weeks after surgery. Patients were further monitored up to 3 years to investigate development of new-onset diabetes mellitus (NODM) in patients without diabetes mellitus (DM) at baseline or worsening of glucose regulation (≥1% increase in glycosylated hemoglobin [HbA1c]) in those with preexisting DM.
Results
The disposition index, an integrated measure of β-cell function, decreased 1 week after surgery in both groups, but it increased more than baseline level in the PD group while its decreased level was maintained in the DP group, resulting in a between-group difference at the 1-year examination (P<0.001). During follow-up, the DP group showed higher incidence of NODM and worsening of glucose regulation than the PD group with hazard ratio (HR) 4.29 (95% confidence interval [CI], 1.49 to 12.3) and HR 2.15 (95% CI, 1.09 to 4.24), respectively, in the multivariate analysis including dynamic glycemic excursion profile. In the DP procedure, distal DP and spleen preservation were associated with better glucose regulation. DP had a stronger association with glucose dysregulation than PD.
Conclusion
Proactive surveillance of glucose dysregulation is advised, particularly for patients who receive DP.
- Drug/Regimen
- Effect of Lactobacillus plantarum LMT1-48 on Body Fat in Overweight Subjects: A Randomized, Double-Blind, Placebo-Controlled Trial
- Minji Sohn, Hyeyoung Jung, Woo Shun Lee, Tai Hoon Kim, Soo Lim
- Diabetes Metab J. 2023;47(1):92-103. Published online April 29, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0370

- 8,891 View
- 383 Download
- 9 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We investigated whether Lactobacillus plantarum strain LMT1-48, isolated from Korean fermented foods and newborn feces, is a suitable probiotic supplement to treat overweight subjects.
Methods
In this randomized, double-blind, placebo-controlled clinical trial, 100 volunteers with a body mass index of 25 to 30 kg/m2 were assigned randomly (1:1) to receive 2×1010 colony forming units of LMT1-48 or to a placebo treatment group. Body composition was measured by dual-energy X-ray absorptiometry, and abdominal visceral fat area (VFA) and subcutaneous fat area were measured by computed tomography scanning. Changes in body fat, VFA, anthropometric parameters, and biomarkers were compared between the two treatment groups (ClinicalTrials.gov number: NCT03759743).
Results
After 12 weeks of treatment, the body weight decreased significantly from 76.6±9.4 to 75.7±9.2 kg in the LMT1-48 group but did not change in the placebo group (P=0.022 between groups). A similar pattern was found in abdominal VFA between the two groups (P=0.041). Serum insulin levels, the corresponding homeostasis model assessment of insulin resistance, and leptin levels decreased in the LMT1-48 group but increased in the placebo group (all P<0.05). Decrease in body weight and body mass index by treatment with LMT1-48 was correlated with increase in Lactobacillus levels significantly. LMT1-48 also increased Oscillibacter levels significantly, which were negatively correlated with triglyceride and alanine transaminase levels.
Conclusion
Administration of LMT1-48 decreased body weight, abdominal VFA, insulin resistance, and leptin levels in these subjects with overweight, suggesting its anti-obesogenic therapeutic potential. -
Citations
Citations to this article as recorded by- Beneficial effects of the probiotics and synbiotics supplementation on anthropometric indices and body composition in adults: A systematic review and meta‐analysis
Saeede Saadati, Kaveh Naseri, Omid Asbaghi, Mohsen Yousefi, Elnaz Golalipour, Barbora de Courten
Obesity Reviews.2024;[Epub] CrossRef - The Effect of Lactobacillus plantarum on the Fecal Microbiota, Short Chain Fatty Acids, Odorous Substances, and Blood Biochemical Indices of Cats
Bing Han, Shukun Liang, Jintao Sun, Hui Tao, Zhenlong Wang, Baosheng Liu, Xiumin Wang, Jie Liu, Jinquan Wang
Microorganisms.2024; 12(1): 91. CrossRef - Natto alleviates hyperlipidemia in high-fat diet-fed mice by modulating the composition and metabolic function of gut microbiota
Le-Yuan Shang, Shuo Zhang, Min Zhang, Xiao-Dong Sun, Qi Wang, Yu-Jie Liu, Yan-Ni Zhao, Mei Zhao, Peng-Jiao Wang, Xiu-Li Gao
Journal of Functional Foods.2024; 112: 105968. CrossRef - Microbial-Based Bioactive Compounds to Alleviate Inflammation in Obesity
Oladayo Emmanuel Apalowo, Grace Adeola Adegoye, Tolulope Mobolaji Obuotor
Current Issues in Molecular Biology.2024; 46(3): 1810. CrossRef - Anti-obesogenic effects of plant natural products: A focus on Korean traditional foods
Gitishree Das, Luis Alfonso Jiménez Ortega, Sandra Gonçalves, J. Basilio Heredia, Maria de Lourdes Gomes Pereira, Anabela Romano, Han-Seung Shin, Jayanta Kumar Patra
Trends in Food Science & Technology.2024; : 104470. CrossRef - A 12-Week, Single-Centre, Randomised, Double-Blind, Placebo-Controlled, Parallel-Design Clinical Trial for the Evaluation of the Efficacy and Safety of Lactiplantibacillus plantarum SKO-001 in Reducing Body Fat
Seon Mi Shin, Jeong-Su Park, Sang Back Kim, Young Hee Cho, Hee Seo, Hak Sung Lee
Nutrients.2024; 16(8): 1137. CrossRef - 3D printing of microencapsulated Lactobacillus rhamnosus for oral delivery
Pablo Rosas-Val, Masoud Adhami, Ana Brotons-Canto, Carlos Gamazo, Juan M. Irache, Eneko Larrañeta
International Journal of Pharmaceutics.2023; 641: 123058. CrossRef - Gut commensal Kineothrix alysoides mitigates liver dysfunction by restoring lipid metabolism and gut microbial balance
Kyoung Jin Choi, Mi Young Yoon, Ji-Eun Kim, Sang Sun Yoon
Scientific Reports.2023;[Epub] CrossRef - Ameliorating Effects of Bifidobacterium longum subsp. infantis FB3-14 against High-Fat-Diet-Induced Obesity and Gut Microbiota Disorder
Ruixin Kou, Jin Wang, Ang Li, Yuanyifei Wang, Bowei Zhang, Jingmin Liu, Yi Sun, Shuo Wang
Nutrients.2023; 15(19): 4104. CrossRef - Effect of Continuous Ingestion of Bifidobacteria and Inulin on Reducing Body Fat: A Randomized, Double-Blind, Placebo-Controlled, Parallel-Group Comparison Study
Yuhei Baba, Yasuo Saito, Mei Kadowaki, Naoki Azuma, Daisuke Tsuge
Nutrients.2023; 15(24): 5025. CrossRef - A Review of the Potential of Probiotic Bacteria in Managing the Body Weight of Obese Individuals
A Didban, L Manafi, R Mahmoudi
Journal of Health and Hygiene.2023; 14(4): 388. CrossRef - Plant-Derived Lactobacillus paracasei IJH-SONE68 Improves the Gut Microbiota Associated with Hepatic Disorders: A Randomized, Double-Blind, and Placebo-Controlled Clinical Trial
Narandalai Danshiitsoodol, Masafumi Noda, Keishi Kanno, Tomoyuki Uchida, Masanori Sugiyama
Nutrients.2022; 14(21): 4492. CrossRef
- Beneficial effects of the probiotics and synbiotics supplementation on anthropometric indices and body composition in adults: A systematic review and meta‐analysis
- Drug/Regimen
- A Real-World Study of Long-Term Safety and Efficacy of Lobeglitazone in Korean Patients with Type 2 Diabetes Mellitus
- Bo-Yeon Kim, Hyuk-Sang Kwon, Suk Kyeong Kim, Jung-Hyun Noh, Cheol-Young Park, Hyeong-Kyu Park, Kee-Ho Song, Jong Chul Won, Jae Myung Yu, Mi Young Lee, Jae Hyuk Lee, Soo Lim, Sung Wan Chun, In-Kyung Jeong, Choon Hee Chung, Seung Jin Han, Hee-Seok Kim, Ju-Young Min, Sungrae Kim
- Diabetes Metab J. 2022;46(6):855-865. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0264
- 6,696 View
- 296 Download
- 6 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Thiazolidinediones (TZDs) have been associated with various safety concerns including weight gain, bladder cancer, and congestive heart failure (CHF). This study evaluated the efficacy and safety of lobeglitazone, a novel TZD in patients with type 2 diabetes mellitus (T2DM) in real practice.
Methods
In this non-interventional, multi-center, retrospective, and observational study conducted at 15 tertiary or secondary referral hospitals in Korea, a total of 2,228 patients with T2DM who received lobeglitazone 0.5 mg for more than 1 year were enrolled.
Results
Overall adverse events (AEs) occurred in 381 patients (17.10%) including edema in 1.97% (n=44). Cerebrovascular and cardiovascular diseases were identified in 0.81% (n=18) and 0.81% (n=18), respectively. One case of CHF was reported as an AE. Edema occurred in 1.97% (n=44) of patients. Hypoglycemia occurred in 2.47% (n=55) of patients. Fracture occurred in 1.17% (n=26) of all patients. Lobeglitazone significantly decreased HbA1c level, resulting in a mean treatment difference of -1.05%± 1.35% (P<0.001), and decreased total cholesterol, triglyceride, and low-density lipoprotein cholesterol. However, it increased high-density lipoprotein cholesterol, regardless of statin administration. The patients who received lobeglitazone 0.5 mg showed an apparent reduction in glycosylated hemoglobin (HbA1c) from baseline during the first 6 months of treatment. The HbA1c levels remained stable between months 6 and 42.
Conclusion
Lobeglitazone has long-term safety profile, good glycemic-lowering effect and long-term durability of glycemic control in real-world clinical settings. -
Citations
Citations to this article as recorded by- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
Deep Dutta, Saptarshi Bhattacharya, Manoj Kumar, Priyankar K. Datta, Ritin Mohindra, Meha Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102697. CrossRef - Efficacy and safety of lobeglitazone, a new Thiazolidinedione, as compared to the standard of care in type 2 diabetes mellitus: A systematic review and meta-analysis
Shashank R. Joshi, Saibal Das, Suja Xaviar, Shambo Samrat Samajdar, Indranil Saha, Sougata Sarkar, Shatavisa Mukherjee, Santanu Kumar Tripathi, Jyotirmoy Pal, Nandini Chatterjee
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102703. CrossRef - Will lobeglitazone rival pioglitazone? A systematic review and critical appraisal
Kalyan Kumar Gangopadhyay, Awadhesh Kumar Singh
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(4): 102747. CrossRef - Lobeglitazone
Reactions Weekly.2023; 1948(1): 262. CrossRef - Lobeglitazone, a novel thiazolidinedione, for secondary prevention in patients with ischemic stroke: a nationwide nested case-control study
Joonsang Yoo, Jimin Jeon, Minyoul Baik, Jinkwon Kim
Cardiovascular Diabetology.2023;[Epub] CrossRef - Lobeglitazone and Its Therapeutic Benefits: A Review
Balamurugan M, Sarumathy S, Robinson R
Cureus.2023;[Epub] CrossRef - Oldies but Goodies: Thiazolidinedione as an Insulin Sensitizer with Cardioprotection
Eun-Hee Cho
Diabetes & Metabolism Journal.2022; 46(6): 827. CrossRef
- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
- Clinical Diabetes & Therapeutics
- Progression to Gestational Diabetes Mellitus in Pregnant Women with One Abnormal Value in Repeated Oral Glucose Tolerance Tests
- Sunyoung Kang, Min Hyoung Kim, Moon Young Kim, Joon-Seok Hong, Soo Heon Kwak, Sung Hee Choi, Soo Lim, Kyong Soo Park, Hak C. Jang
- Diabetes Metab J. 2019;43(5):607-614. Published online February 28, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0159
- 5,879 View
- 103 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Women with one abnormal value (OAV) in a 100 g oral glucose tolerance test (OGTT) during pregnancy are reported to have an increased risk of adverse pregnancy outcomes. However, there is limited data about whether women with OAV will progress to gestational diabetes mellitus (GDM) when the OGTT is repeated.
Methods To identify clinical and metabolic predictors for GDM in women with OAV, we conducted a retrospective study and identified women with OAV in the OGTT done at 24 to 30 weeks gestational age (GA) and repeated the second OGTT between 32 and 34 weeks of GA.
Results Among 137 women with OAV in the initial OGTT, 58 (42.3%) had normal, 40 (29.2%) had OAV and 39 (28.5%) had GDM in the second OGTT. Maternal age, prepregnancy body mass index, weight gain from prepregnancy to the second OGTT, GA at the time of the OGTT, and parity were similar among normal, OAV, and GDM groups. Plasma glucose levels in screening tests were different (151.8±15.7, 155.8±14.6, 162.5±20.3 mg/dL,
P <0.05), but fasting, 1-, 2-, and 3-hour glucose levels in the initial OGTT were not. Compared to women with screen negative, women with untreated OAV had a higher frequency of macrosomia.Conclusion We demonstrated that women with OAV in the initial OGTT significantly progressed to GDM in the second OGTT. Clinical parameters predicting progression to GDM were not found. Repeating the OGTT in women with OAV in the initial test may be helpful to detect GDM progression.
-
Citations
Citations to this article as recorded by- Maternal and fetal outcomes of pregnancies associated with single versus double abnormal values in 100 gr glucose tolerance test
Mohammadali Shahriari, Ali Shahriari, Maryam Khooshideh, Anahita Dehghaninezhad, Arezoo Maleki-Hajiagha, Rana Karimi
Journal of Diabetes & Metabolic Disorders.2023; 22(2): 1347. CrossRef - One abnormal value or vomiting after oral glucose tolerance test in pregnancy: incidence and impact on maternal-fetal outcomes
Humberto Navarro-Martinez, Juana-Antonia Flores-Le Roux, Gemma Llauradó, Lucia Gortazar, Antonio Payà, Laura Mañé, Juan Pedro-Botet, David Benaiges
Gynecological Endocrinology.2023;[Epub] CrossRef - Analysis of the gut microflora in women with gestational diabetes mellitus
Xuping Wang, Bingfeng Bian, Fuman Du, Chaofeng Xiang, Yu Liu, Na Li, Binhong Duan
International Journal of Diabetes in Developing Countries.2023;[Epub] CrossRef - The association between gestational impaired glucose tolerance and hyperglycemic markers: A prospective study
Ohad Gluck, Hadas Ganer Herman, Nataly Fainstein, Neri Katz, Jacob Bar, Michal Kovo
International Journal of Gynecology & Obstetrics.2022; 156(1): 82. CrossRef - Association of abnormal-glucose tolerance during pregnancy with exposure to PM2.5 components and sources
Dejian Mai, Chengfang Xu, Weiwei Lin, Dingli Yue, Shaojie Fu, Jianqing Lin, Luan Yuan, Yan Zhao, Yuhong Zhai, Huiying Mai, Xiaoling Zeng, Tingwu Jiang, Xuejiao Li, Jiajia Dai, Boning You, Qin Xiao, Qing Wei, Qiansheng Hu
Environmental Pollution.2022; 292: 118468. CrossRef - Postprandial Free Fatty Acids at Mid-Pregnancy Increase the Risk of Large-for-Gestational-Age Newborns in Women with Gestational Diabetes Mellitus
So-Yeon Kim, Young Shin Song, Soo-Kyung Kim, Yong-Wook Cho, Kyung-Soo Kim
Diabetes & Metabolism Journal.2022; 46(1): 140. CrossRef - The Clinical Characteristics of Gestational Diabetes Mellitus in Korea: A National Health Information Database Study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Endocrinology and Metabolism.2021; 36(3): 628. CrossRef - Gestational Diabetes Mellitus: Diagnosis and Glycemic Control
Tae Jung Oh, Hak Chul Jang
The Journal of Korean Diabetes.2020; 21(2): 69. CrossRef - Health literacy and diabetes control in pregnant women
Azar Pirdehghan, Mohammad Eslahchi, Farzaneh Esna-Ashari, Shiva Borzouei
Journal of Family Medicine and Primary Care.2020; 9(2): 1048. CrossRef
- Maternal and fetal outcomes of pregnancies associated with single versus double abnormal values in 100 gr glucose tolerance test
- Epidemiology
- Oral Glucose Tolerance Testing Allows Better Prediction of Diabetes in Women with a History of Gestational Diabetes Mellitus
- Tae Jung Oh, Yeong Gi Kim, Sunyoung Kang, Joon Ho Moon, Soo Heon Kwak, Sung Hee Choi, Soo Lim, Kyong Soo Park, Hak C. Jang, Joon-Seok Hong, Nam H. Cho
- Diabetes Metab J. 2019;43(3):342-349. Published online December 7, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0086
- 4,680 View
- 59 Download
- 10 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We aimed to identify the postpartum metabolic factors that were associated with the development of diabetes in women with a history of gestational diabetes mellitus (GDM). In addition, we examined the role of the oral glucose tolerance test (OGTT) in the prediction of future diabetes.
Methods We conducted a prospective study of 179 subjects who previously had GDM but did not have diabetes at 2 months postpartum. The initial postpartum examination including a 75-g OGTT and the frequently sampled intravenous glucose tolerance test (FSIVGTT) was performed 12 months after delivery, and annual follow-up visits were made thereafter.
Results The insulinogenic index (IGI30) obtained from the OGTT was significantly correlated with the acute insulin response to glucose (AIRg) obtained from the FSIVGTT. The disposition indices obtained from the OGTT and FSIVGTT were also significantly correlated. Women who progressed to diabetes had a lower insulin secretory capacity including IGI30, AIRg, and disposition indices obtained from the FSIVGTT and OGTT compared with those who did not. However, the insulin sensitivity indices obtained from the OGTT and FSIVGTT did not differ between the two groups. Multivariate logistic regression analysis showed that the 2-hour glucose and disposition index obtained from the FSIVGTT were significant postpartum metabolic risk factors for the development of diabetes.
Conclusion We identified a crucial role of β-cell dysfunction in the development of diabetes in Korean women with previous GDM. The 2-hour glucose result from the OGTT is an independent predictor of future diabetes. Therefore, the OGTT is crucial for better prediction of future diabetes in Korean women with previous GDM.
-
Citations
Citations to this article as recorded by- Diagnosis and management of gestational diabetes mellitus
Tae Jung Oh
Journal of the Korean Medical Association.2023; 66(7): 414. CrossRef - Risk factors for women with gestational diabetes mellitus developing type 2 diabetes and the impact on children's health
Yi‐Ling Chiou, Chich‐Hsiu Hung, Ching‐Yun Yu, Te‐Fu Chan, Ming‐Gwo Liu
Journal of Clinical Nursing.2022; 31(7-8): 1005. CrossRef - Postprandial Free Fatty Acids at Mid-Pregnancy Increase the Risk of Large-for-Gestational-Age Newborns in Women with Gestational Diabetes Mellitus
So-Yeon Kim, Young Shin Song, Soo-Kyung Kim, Yong-Wook Cho, Kyung-Soo Kim
Diabetes & Metabolism Journal.2022; 46(1): 140. CrossRef - Gestational Diabetes Mellitus: Diagnostic Approaches and Maternal-Offspring Complications
Joon Ho Moon, Hak Chul Jang
Diabetes & Metabolism Journal.2022; 46(1): 3. CrossRef - Higher Muscle Mass Protects Women with Gestational Diabetes Mellitus from Progression to Type 2 Diabetes Mellitus
Yujin Shin, Joon Ho Moon, Tae Jung Oh, Chang Ho Ahn, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
Diabetes & Metabolism Journal.2022; 46(6): 890. CrossRef - Pancreatic fat accumulation is associated with decreased β‐cell function and deterioration in glucose tolerance in Korean adults
Sang Ouk Chin, You‐Cheol Hwang, In‐Jin Cho, In‐Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung
Diabetes/Metabolism Research and Reviews.2021;[Epub] CrossRef - The Clinical Characteristics of Gestational Diabetes Mellitus in Korea: A National Health Information Database Study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Endocrinology and Metabolism.2021; 36(3): 628. CrossRef - Bihormonal dysregulation of insulin and glucagon contributes to glucose intolerance development at one year post-delivery in women with gestational diabetes: a prospective cohort study using an early postpartum 75-g glucose tolerance test
Riyoko Shigeno, Ichiro Horie, Masaki Miwa, Ayako Ito, Ai Haraguchi, Shoko Natsuda, Satoru Akazawa, Ai Nagata, Yuri Hasegawa, Shoko Miura, Kiyonori Miura, Atsushi Kawakami, Norio Abiru
Endocrine Journal.2021; 68(8): 919. CrossRef - Risk factors during the early postpartum period for type 2 diabetes mellitus in women with gestational diabetes
Maki Kawasaki, Naoko Arata, Naoko Sakamoto, Anna Osamura, Siori Sato, Yoshihiro Ogawa, Ichiro Yasuhi, Masako Waguri, Yuji Hiramatsu
Endocrine Journal.2020; 67(4): 427. CrossRef - Cod-Liver Oil Improves Metabolic Indices and hs-CRP Levels in Gestational Diabetes Mellitus Patients: A Double-Blind Randomized Controlled Trial
Shuli Yang, Ruixin Lin, Lihui Si, Zhuo Li, Wenwen Jian, Qing Yu, Yan Jia
Journal of Diabetes Research.2019; 2019: 1. CrossRef
- Diagnosis and management of gestational diabetes mellitus
- Clinical Diabetes & Therapeutics
- Effects of Lobeglitazone, a Novel Thiazolidinedione, on Bone Mineral Density in Patients with Type 2 Diabetes Mellitus over 52 Weeks
- Soo Lim, Kyoung Min Kim, Sin Gon Kim, Doo Man Kim, Jeong-Taek Woo, Choon Hee Chung, Kyung Soo Ko, Jeong Hyun Park, Yongsoo Park, Sang Jin Kim, Hak Chul Jang, Dong Seop Choi
- Diabetes Metab J. 2017;41(5):377-385. Published online October 24, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.5.377
- 4,260 View
- 42 Download
- 19 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aim of this multicenter, randomized, double-blind study was to examine the effect of lobeglitazone, a novel thiazolidinedione, on the changes in bone mineral density (BMD) in patients with type 2 diabetes mellitus.
Methods A 24-week, double-blinded phase was followed by a 28-week, open-label phase, in which the placebo group also started to receive lobeglitazone. A total of 170 patients aged 34 to 76 years were randomly assigned in a 2:1 ratio to receive lobeglitazone 0.5 mg or a matching placebo orally, once daily. BMD was assessed using dual-energy X-ray absorptiometry at week 24 and at the end of the study (week 52).
Results During the double-blinded phase, the femur neck BMD showed decreasing patterns in both groups, without statistical significance (−0.85%±0.36% and −0.78%±0.46% in the lobeglitazone and placebo groups, respectively). The treatment difference between the groups was 0.07%, which was also not statistically significant. Further, minimal, nonsignificant decreases were observed in both groups in the total hip BMD compared to values at baseline, and these differences also did not significantly differ between the groups. During the open-label phase, the BMD was further decreased, but not significantly, by −0.32% at the femur neck and by −0.60% at the total hip in the lobeglitazone group, and these changes did not significantly differ compared with the original placebo group switched to lobeglitazone.
Conclusion Our results indicate that treatment with lobeglitazone 0.5 mg over 52 weeks showed no detrimental effect on the BMD compared to the placebo.
-
Citations
Citations to this article as recorded by- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
Deep Dutta, Saptarshi Bhattacharya, Manoj Kumar, Priyankar K. Datta, Ritin Mohindra, Meha Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102697. CrossRef - Efficacy and safety of lobeglitazone, a new Thiazolidinedione, as compared to the standard of care in type 2 diabetes mellitus: A systematic review and meta-analysis
Shashank R. Joshi, Saibal Das, Suja Xaviar, Shambo Samrat Samajdar, Indranil Saha, Sougata Sarkar, Shatavisa Mukherjee, Santanu Kumar Tripathi, Jyotirmoy Pal, Nandini Chatterjee
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102703. CrossRef - The benefits of adipocyte metabolism in bone health and regeneration
Lisa-Marie Burkhardt, Christian H. Bucher, Julia Löffler, Charlotte Rinne, Georg N. Duda, Sven Geissler, Tim J. Schulz, Katharina Schmidt-Bleek
Frontiers in Cell and Developmental Biology.2023;[Epub] CrossRef - Will lobeglitazone rival pioglitazone? A systematic review and critical appraisal
Kalyan Kumar Gangopadhyay, Awadhesh Kumar Singh
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(4): 102747. CrossRef - Comparison of therapeutic efficacy and safety of sitagliptin, dapagliflozin, or lobeglitazone adjunct therapy in patients with type 2 diabetes mellitus inadequately controlled on sulfonylurea and metformin: Third agent study
Jun Hwa Hong, Jun Sung Moon, Kayeon Seong, Soo Lim
Diabetes Research and Clinical Practice.2023; 203: 110872. CrossRef - Bone Mineral Density Evaluation Among Type 2 Diabetic Patients in Rural Haryana, India: An Analytical Cross-Sectional Study
Nitish Khandelwal, Surbhi Rajauria, Siddhesh Pandurang Kanjalkar, Omkar Shivaji Chavanke, Sanjay Rai
Cureus.2023;[Epub] CrossRef - Lobeglitazone and Its Therapeutic Benefits: A Review
Balamurugan M, Sarumathy S, Robinson R
Cureus.2023;[Epub] CrossRef - A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - A Real-World Study of Long-Term Safety and Efficacy of Lobeglitazone in Korean Patients with Type 2 Diabetes Mellitus
Bo-Yeon Kim, Hyuk-Sang Kwon, Suk Kyeong Kim, Jung-Hyun Noh, Cheol-Young Park, Hyeong-Kyu Park, Kee-Ho Song, Jong Chul Won, Jae Myung Yu, Mi Young Lee, Jae Hyuk Lee, Soo Lim, Sung Wan Chun, In-Kyung Jeong, Choon Hee Chung, Seung Jin Han, Hee-Seok Kim, Ju-Y
Diabetes & Metabolism Journal.2022; 46(6): 855. CrossRef - Comparative Efficacy of Lobeglitazone Versus Pioglitazone on Albuminuria in Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes Therapy.2021; 12(1): 171. CrossRef - Lobeglitazone: A Novel Thiazolidinedione for the Management of Type 2 Diabetes Mellitus
Jaehyun Bae, Taegyun Park, Hyeyoung Kim, Minyoung Lee, Bong-Soo Cha
Diabetes & Metabolism Journal.2021; 45(3): 326. CrossRef - Effect of lobeglitazone on motor function in rat model of Parkinson’s disease with diabetes co-morbidity
Kambiz Hassanzadeh, Arman Rahimmi, Mohammad Raman Moloudi, Rita Maccarone, Massimo Corbo, Esmael Izadpanah, Marco Feligioni
Brain Research Bulletin.2021; 173: 184. CrossRef - Recent Perspective on Thiazolidinedione
Won Jun Kim
The Journal of Korean Diabetes.2021; 22(2): 97. CrossRef - Use of in vitro bone models to screen for altered bone metabolism, osteopathies, and fracture healing: challenges of complex models
Sabrina Ehnert, Helen Rinderknecht, Romina H. Aspera-Werz, Victor Häussling, Andreas K. Nussler
Archives of Toxicology.2020; 94(12): 3937. CrossRef - Update on: effects of anti-diabetic drugs on bone metabolism
Guillaume Mabilleau, Béatrice Bouvard
Expert Review of Endocrinology & Metabolism.2020; 15(6): 415. CrossRef - The use of metformin, insulin, sulphonylureas, and thiazolidinediones and the risk of fracture: Systematic review and meta‐analysis of observational studies
Khemayanto Hidayat, Xuan Du, Meng‐Jiao Wu, Bi‐Min Shi
Obesity Reviews.2019; 20(10): 1494. CrossRef - Diabetes pharmacotherapy and effects on the musculoskeletal system
Evangelia Kalaitzoglou, John L. Fowlkes, Iuliana Popescu, Kathryn M. Thrailkill
Diabetes/Metabolism Research and Reviews.2019;[Epub] CrossRef - Morin Exerts Anti‐Arthritic Effects by Attenuating Synovial Angiogenesis via Activation of Peroxisome Proliferator Activated Receptor‐γ
Mengfan Yue, Ni Zeng, Yufeng Xia, Zhifeng Wei, Yue Dai
Molecular Nutrition & Food Research.2018;[Epub] CrossRef - The effects of diabetes therapy on bone: A clinical perspective
Karim G. Kheniser, Carmen M. Polanco Santos, Sangeeta R. Kashyap
Journal of Diabetes and its Complications.2018; 32(7): 713. CrossRef - Changes in the Bone Mineral Density of Femur Neck and Total Hip Over a 52-Week Treatment with Lobeglitazone
Da Young Lee, Ji A Seo
Diabetes & Metabolism Journal.2017; 41(5): 374. CrossRef
- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
- Obesity and Metabolic Syndrome
- Relationship between Regional Body Fat Distribution and Diabetes Mellitus: 2008 to 2010 Korean National Health and Nutrition Examination Surveys
- Soo In Choi, Dawn Chung, Jung Soo Lim, Mi Young Lee, Jang Yel Shin, Choon Hee Chung, Ji Hye Huh
- Diabetes Metab J. 2017;41(1):51-59. Published online December 21, 2016
- DOI: https://doi.org/10.4093/dmj.2017.41.1.51
- 4,167 View
- 42 Download
- 35 Web of Science
- 36 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aim of this study was to investigate the association between regional body fat distribution, especially leg fat mass, and the prevalence of diabetes mellitus (DM) in adult populations.
Methods A total of 3,181 men and 3,827 postmenopausal women aged 50 years or older were analyzed based on Korea National Health and Nutrition Examination Surveys (2008 to 2010). Body compositions including muscle mass and regional fat mass were measured using dual-energy X-ray absorptiometry.
Results The odds ratios (ORs) for DM was higher with increasing truncal fat mass and arm fat mass, while it was lower with increasing leg fat mass. In a partial correlation analysis adjusted for age, leg fat mass was negatively associated with glycosylated hemoglobin in both sexes and fasting glucose in women. Leg fat mass was positively correlated with appendicular skeletal muscle mass and homeostasis model assessment of β cell. In addition, after adjusting for confounding factors, the OR for DM decreased gradually with increasing leg fat mass quartiles in both genders. When we subdivided the participants into four groups based on the median values of leg fat mass and leg muscle mass, higher leg fat mass significantly lowered the risk of DM even though they have smaller leg muscle mass in both genders (
P <0.001).Conclusion The relationship between fat mass and the prevalence of DM is different according to regional body fat distribution. Higher leg fat mass was associated with a lower risk of DM in Korean populations. Maintaining leg fat mass may be important in preventing impaired glucose tolerance.
-
Citations
Citations to this article as recorded by- Effects of chromium supplementation on body composition in patients with type 2 diabetes: A dose-response systematic review and meta-analysis of randomized controlled trials
Mahdi Vajdi, Mahsa khajeh, Ehsan Safaei, Seyedehelham Moeinolsadat, Samin Mousavi, Hooria Seyedhosseini-Ghaheh, Mahdieh Abbasalizad-Farhangi, Gholamreza Askari
Journal of Trace Elements in Medicine and Biology.2024; 81: 127338. CrossRef - Connections between body composition and dysregulation of islet α- and β-cells in type 2 diabetes
Jia-xi Miao, Jia-ping Xu, Rui Wang, Yu-xian Xu, Feng Xu, Chun-hua Wang, Chao Yu, Dong-mei Zhang, Jian-bin Su
Diabetology & Metabolic Syndrome.2024;[Epub] CrossRef - Anthropometric and DXA-derived measures of body composition in relation to pre-diabetes among adults
Anwar Mohammad, Ali H. Ziyab, Talal Mohammad
BMJ Open Diabetes Research & Care.2023; 11(5): e003412. CrossRef - A cohort study on the predictive capability of body composition for diabetes mellitus using machine learning
Mohammad Ali Nematollahi, Amir Askarinejad, Arefeh Asadollahi, Mehdi Bazrafshan, Shirin Sarejloo, Mana Moghadami, Sarvin Sasannia, Mojtaba Farjam, Reza Homayounfar, Babak Pezeshki, Mitra Amini, Mohamad Roshanzamir, Roohallah Alizadehsani, Hanieh Bazrafsha
Journal of Diabetes & Metabolic Disorders.2023;[Epub] CrossRef - Which is the best diet to reduce cardiometabolic risk: dietary counseling or home-delivered diet?
Feray Çağiran Yilmaz, Aysun Atilgan, Günay Saka
Food & Nutrition Research.2023;[Epub] CrossRef - Sedentary lifestyle and body composition in type 2 diabetes
Dan-dan Li, Yang Yang, Zi-yi Gao, Li-hua Zhao, Xue Yang, Feng Xu, Chao Yu, Xiu-lin Zhang, Xue-qin Wang, Li-hua Wang, Jian-bin Su
Diabetology & Metabolic Syndrome.2022;[Epub] CrossRef - Impaired Lung Function and Lung Cancer Incidence: A Nationwide Population-Based Cohort Study
Hye Seon Kang, Yong-Moon Park, Seung-Hyun Ko, Seung Hoon Kim, Shin Young Kim, Chi Hong Kim, Kyungdo Han, Sung Kyoung Kim
Journal of Clinical Medicine.2022; 11(4): 1077. CrossRef - Association between lung function and the risk of atrial fibrillation in a nationwide population cohort study
Su Nam Lee, Seung-Hyun Ko, Sung-Ho Her, Kyungdo Han, Donggyu Moon, Sung Kyoung Kim, Ki-Dong Yoo, Yu-Bae Ahn
Scientific Reports.2022;[Epub] CrossRef - Is imaging-based muscle quantity associated with risk of diabetes? A meta-analysis of cohort studies
Shanhu Qiu, Xue Cai, Yang Yuan, Bo Xie, Zilin Sun, Tongzhi Wu
Diabetes Research and Clinical Practice.2022; 189: 109939. CrossRef - Research Progress of Body Composition Changes in Type 2 Diabetes Patients
鹏霞 张
Advances in Clinical Medicine.2022; 12(08): 7181. CrossRef - Associations of eating speed with fat distribution and body shape vary in different age groups and obesity status
Saili Ni, Menghan Jia, Xuemiao Wang, Yun Hong, Xueyin Zhao, Liang Zhang, Yuan Ru, Fei Yang, Shankuan Zhu
Nutrition & Metabolism.2022;[Epub] CrossRef - Body composition, trabecular bone score and vertebral fractures in subjects with Klinefelter syndrome
W. Vena, F. Carrone, A. Delbarba, O. Akpojiyovbi, L. C. Pezzaioli, P. Facondo, C. Cappelli, L. Leonardi, L. Balzarini, D. Farina, A. Pizzocaro, A. G. Lania, G. Mazziotti, A. Ferlin
Journal of Endocrinological Investigation.2022; 46(2): 297. CrossRef - Genetically predicted body fat mass and distribution with diabetic kidney disease: A two-sample Mendelian randomization study
Min Wang, Xin Li, Hang Mei, Zhao-Hui Huang, Yue Liu, Yong-Hong Zhu, Tian-Kui Ma, Qiu-Ling Fan
Frontiers in Genetics.2022;[Epub] CrossRef - Screening for Prediabetes and Diabetes in Korean Nonpregnant Adults: A Position Statement of the Korean Diabetes Association, 2022
Kyung Ae Lee, Dae Jung Kim, Kyungdo Han, Suk Chon, Min Kyong Moon
Diabetes & Metabolism Journal.2022; 46(6): 819. CrossRef - Age- and Sex-Related Differential Associations between Body Composition and Diabetes Mellitus
Eun Roh, Soon Young Hwang, Jung A Kim, You-Bin Lee, So-hyeon Hong, Nam Hoon Kim, Ji A Seo, Sin Gon Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
Diabetes & Metabolism Journal.2021; 45(2): 183. CrossRef - Neck circumference and metabolic syndrome: A cross-sectional population-based study
Hooman Ebrahimi, Payam Mahmoudi, Farhad Zamani, Sedighe Moradi
Primary Care Diabetes.2021; 15(3): 582. CrossRef - Development of a clinical risk score for incident diabetes: A 10‐year prospective cohort study
Tae Jung Oh, Jae Hoon Moon, Sung Hee Choi, Young Min Cho, Kyong Soo Park, Nam H Cho, Hak Chul Jang
Journal of Diabetes Investigation.2021; 12(4): 610. CrossRef - The association of glucocorticoid receptor polymorphism with metabolic outcomes in menopausal women with adrenal incidentalomas
Sanja Ognjanović, Jadranka Antić, Tatjana Pekmezović, Bojana Popović, Tatjana Isailović, Ivana Božić Antić, Tamara Bogavac, Valentina Elezović Kovačević, Dušan Ilić, Milica Opalić, Djuro Macut
Maturitas.2021; 151: 15. CrossRef - Distinct opposing associations of upper and lower body fat depots with metabolic and cardiovascular disease risk markers
Mahasampath Gowri S, Belavendra Antonisamy, Finney S. Geethanjali, Nihal Thomas, Felix Jebasingh, Thomas V. Paul, Fredrik Karpe, Clive Osmond, Caroline H. D. Fall, Senthil K. Vasan
International Journal of Obesity.2021; 45(11): 2490. CrossRef - Body Roundness Index Is a Superior Obesity Index in Predicting Diabetes Risk Among Hypertensive Patients: A Prospective Cohort Study in China
Yingshan Liu, Xiaocong Liu, Haixia Guan, Shuting Zhang, Qibo Zhu, Xiaoying Fu, Hongmei Chen, Songtao Tang, Yingqing Feng, Jian Kuang
Frontiers in Cardiovascular Medicine.2021;[Epub] CrossRef - Subcutaneous adipose tissue distribution and serum lipid/lipoprotein in unmedicated postmenopausal women: A B-mode ultrasound study
Imaging.2021; 13(2): 119. CrossRef - The Leg Fat to Total Fat Ratio Is Associated with Lower Risks of Non-Alcoholic Fatty Liver Disease and Less Severe Hepatic Fibrosis: Results from Nationwide Surveys (KNHANES 2008–2011)
Hyun Min Kim, Yong-ho Lee
Endocrinology and Metabolism.2021; 36(6): 1232. CrossRef Optimal Cut-Offs of Body Mass Index and Waist Circumference to Identify Obesity in Chinese Type 2 Diabetic Patients
Qinying Zhao, Xiangjun Chen, Jinshan Wu, Lilin Gong, Jinbo Hu, Shumin Yang, Qifu Li, Zhihong Wang
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 1899. CrossRef- Weight Loss after 12 Weeks of Exercise and/or Nutritional Guidance Is Not Obligatory for Induced Changes in Local Fat/Lean Mass Indexes in Adults with Excess of Adiposity
Robinson Ramírez-Vélez, Mikel Izquierdo, Karem Castro-Astudillo, Carolina Medrano-Mena, Angela Liliana Monroy-Díaz, Rocío del Pilar Castellanos-Vega, Héctor Reynaldo Triana-Reina, María Correa-Rodríguez
Nutrients.2020; 12(8): 2231. CrossRef - VISCERAL FAT, PHYSICAL FITNESS AND BIOCHEMICAL MARKERS OF BRAZILIAN MILITARY PERSONNEL
Laércio Camilo Rodrigues, Marcos de Sá Rego Fortes, Marco Antônio Muniz Lippert, Samir Ezequiel Da Rosa, José Fernandes Filho
Revista Brasileira de Medicina do Esporte.2020; 26(1): 21. CrossRef - Comparison of 7-site skinfold measurement and dual-energy X-ray absorptiometry for estimating body fat percentage and regional adiposity in Taiwanese diabetic patients
Feng-Chih Kuo, Chieh-Hua Lu, Li-Wei Wu, Tung-Wei Kao, Sheng-Chiang Su, Jhih-Syuan Liu, Kuan-Chan Chen, Chia-Hao Chang, Chih-Chun Kuo, Chien-Hsing Lee, Chang-Hsun Hsieh, Mauro Lombardo
PLOS ONE.2020; 15(7): e0236323. CrossRef - Outcomes specific to patient sex after open ventral hernia repair
Kathryn A. Schlosser, Sean R. Maloney, Otto Thielan, Tanushree Prasad, Kent Kercher, Paul D. Colavita, B Todd Heniford, Vedra A. Augenstein
Surgery.2020; 167(3): 614. CrossRef Age-Related Changes in Body Composition and Bone Mineral Density and Their Relationship with the Duration of Diabetes and Glycaemic Control in Type 2 Diabetes
Ying Tang, Lilin Gong, Xiangjun Chen, Zhipeng Du, Jinbo Hu, Zhixin Xu, Jinshan Wu, Qifu Li, Zhihong Wang
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 4699. CrossRef- Lipodystrophy: A paradigm for understanding the consequences of "overloading" adipose tissue
Koini Lim, Afreen Haider, Claire Adams, Alison Sleigh, David Savage
Physiological Reviews.2020;[Epub] CrossRef - Premeal Consumption of a Protein-Enriched, Dietary Fiber-Fortified Bar Decreases Total Energy Intake in Healthy Individuals
Chang Ho Ahn, Jae Hyun Bae, Young Min Cho
Diabetes & Metabolism Journal.2019; 43(6): 879. CrossRef - Differences in dietary intakes, body compositions, and biochemical indices between metabolically healthy and metabolically abnormal obese Korean women
Eun Yeong Kang, Jung-Eun Yim
Nutrition Research and Practice.2019; 13(6): 488. CrossRef - The Association between Body Composition using Dual energy X-ray Absorptiometry and Type-2 Diabetes: A Systematic Review and Meta-Analysis of Observational studies
Preeti Gupta, Carla Lanca, Alfred T. L. Gan, Pauline Soh, Sahil Thakur, Yijin Tao, Neelam Kumari, Ryan E. K. Man, Eva K. Fenwick, Ecosse L. Lamoureux
Scientific Reports.2019;[Epub] CrossRef - Genes that make you fat, but keep you healthy
R. J. F. Loos, T. O. Kilpeläinen
Journal of Internal Medicine.2018; 284(5): 450. CrossRef - Overview of Epidemiology and Contribution of Obesity and Body Fat Distribution to Cardiovascular Disease: An Update
Marie-Eve Piché, Paul Poirier, Isabelle Lemieux, Jean-Pierre Després
Progress in Cardiovascular Diseases.2018; 61(2): 103. CrossRef - Relevance of human fat distribution on lipid and lipoprotein metabolism and cardiovascular disease risk
Marie-Eve Piché, Senthil K. Vasan, Leanne Hodson, Fredrik Karpe
Current Opinion in Lipidology.2018; 29(4): 285. CrossRef - Comparison of regional fat measurements by dual-energy X-ray absorptiometry and conventional anthropometry and their association with markers of diabetes and cardiovascular disease risk
S K Vasan, C Osmond, D Canoy, C Christodoulides, M J Neville, C Di Gravio, C H D Fall, F Karpe
International Journal of Obesity.2018; 42(4): 850. CrossRef
- Effects of chromium supplementation on body composition in patients with type 2 diabetes: A dose-response systematic review and meta-analysis of randomized controlled trials
- Epidemiology
- Application of the 2013 American College of Cardiology/American Heart Association Cholesterol Guideline to the Korean National Health and Nutrition Examination Surveys from 1998 to 2012
- Young Shin Song, Tae Jung Oh, Kyoung Min Kim, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang, Kyong Soo Park, Soo Lim
- Diabetes Metab J. 2017;41(1):38-50. Published online December 16, 2016
- DOI: https://doi.org/10.4093/dmj.2017.41.1.38
- 4,269 View
- 29 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background The 2013 American College of Cardiology/American Heart Association (ACC/AHA) guideline for the treatment of blood cholesterol recommends statin therapy for individuals at high risk of atherosclerotic cardiovascular disease (ASCVD). The aim of this study was to investigate serial trends in the percentages of Korean adults considered eligible for statin therapy according to the new ACC/AHA cholesterol guideline.
Methods Data from the Korean National Health and Nutrition Examination Survey (KNHANES) I (1998,
n =7,698), II (2001,n =5,654), III (2005,n =5,269), IV (2007 to 2009,n =15,727), and V (2010 to 2012,n =16,304), which used a stratified, multistage, probability sampling design, were used as representative of the entire Korean population.Results The percentage of adults eligible for statin therapy according to the ACC/AHA cholesterol guideline increased with time: 17.0%, 19.0%, 20.8%, 20.2%, and 22.0% in KNHANES I, II, III, IV, and V, respectively (
P =0.022). The prevalence of ASCVD was 1.4% in KNHANES I and increased to 3.3% in KNHANES V. The percentage of diabetic patients aged 40 to 75 years with a low density lipoprotein cholesterol levels of 70 to 189 mg/dL increased from 4.8% in KNHANES I to 6.1% in KNHANES V. People with an estimated 10-year ASCVD risk ≥7.5% and aged 40 to 75 years accounted for the largest percentage among the four statin benefit groups: 9.1% in KNHANES I and 11.0% in KNHANES V.Conclusion Application of the 2013 ACC/AHA guideline has found that the percentage of Korean adults in the statin benefit groups has increased over the past 15 years.
-
Citations
Citations to this article as recorded by- Sex differences in risk factors for subclinical hypothyroidism
Jeonghoon Ha, Jeongmin Lee, Kwanhoon Jo, Dong-Jun Lim, Moo Il Kang, Bong Yun Cha, Min-Hee Kim
Endocrine Connections.2018; 7(4): 511. CrossRef
- Sex differences in risk factors for subclinical hypothyroidism
- Others
- Rg3 Improves Mitochondrial Function and the Expression of Key Genes Involved in Mitochondrial Biogenesis in C2C12 Myotubes
- Min Joo Kim, Young Do Koo, Min Kim, Soo Lim, Young Joo Park, Sung Soo Chung, Hak C. Jang, Kyong Soo Park
- Diabetes Metab J. 2016;40(5):406-413. Published online August 12, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.5.406
- 4,904 View
- 71 Download
- 21 Web of Science
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Panax ginseng has glucose-lowering effects, some of which are associated with the improvement in insulin resistance in skeletal muscle. Because mitochondria play a pivotal role in the insulin resistance of skeletal muscle, we investigated the effects of the ginsenoside Rg3, one of the active components ofP. ginseng , on mitochondrial function and biogenesis in C2C12 myotubes.Methods C2C12 myotubes were treated with Rg3 for 24 hours. Insulin signaling pathway proteins were examined by Western blot. Cellular adenosine triphosphate (ATP) levels and the oxygen consumption rate were measured. The protein or mRNA levels of mitochondrial complexes were evaluated by Western blot and quantitative reverse transcription polymerase chain reaction analysis.
Results Rg3 treatment to C2C12 cells activated the insulin signaling pathway proteins, insulin receptor substrate-1 and Akt. Rg3 increased ATP production and the oxygen consumption rate, suggesting improved mitochondrial function. Rg3 increased the expression of peroxisome proliferator-activated receptor γ coactivator 1α, nuclear respiratory factor 1, and mitochondrial transcription factor, which are transcription factors related to mitochondrial biogenesis. Subsequent increased expression of mitochondrial complex IV and V was also observed.
Conclusion Our results suggest that Rg3 improves mitochondrial function and the expression of key genes involved in mitochondrial biogenesis, leading to an improvement in insulin resistance in skeletal muscle. Rg3 may have the potential to be developed as an anti-hyperglycemic agent.
-
Citations
Citations to this article as recorded by- Comparison of Ginseng Leaf Extract and Its Acid-Treated Form, UG0712 Between Their Effects on Exercise Performance in Mice
Young Jin Lee, Su Hyun Yu, Gwang Yeong Seok, Su Yeon Kim, Mi Jeong Kim, Inhye Jeong, Wan Heo, Bo Su Lee, Seon Gil Do, Bok Kyung Han, Young Jun Kim
Food Supplements and Biomaterials for Health.2024;[Epub] CrossRef - Ginsenosides for the treatment of insulin resistance and diabetes: Therapeutic perspectives and mechanistic insights
Tae Hyun Kim
Journal of Ginseng Research.2024; 48(3): 276. CrossRef - Preparation and bioactivity of the rare ginsenosides Rg3 and Rh2: An updated review
Wenqi Xu, Wei Lyu, Cuicui Duan, Fumin Ma, Xiaolei Li, Dan Li
Fitoterapia.2023; 167: 105514. CrossRef - Ginsenoside Rc, an Active Component of Panax ginseng, Alleviates Oxidative Stress-Induced Muscle Atrophy via Improvement of Mitochondrial Biogenesis
Aeyung Kim, Sang-Min Park, No Soo Kim, Haeseung Lee
Antioxidants.2023; 12(8): 1576. CrossRef - Ginsenoside Rg3 protects glucocorticoid‑induced muscle atrophy in vitro through improving mitochondrial biogenesis and myotube growth
Ryuni Kim, Jee Kim, Sang-Jin Lee, Gyu-Un Bae
Molecular Medicine Reports.2022;[Epub] CrossRef - Beneficial Effects of Walnut Oligopeptides on Muscle Loss in Senescence-Accelerated Mouse Prone-8 (SAMP8) Mice: Focusing on Mitochondrial Function
Rui Fan, Yuntao Hao, Qian Du, Jiawei Kang, Meihong Xu, Yong Li
Nutrients.2022; 14(10): 2051. CrossRef - Ginseng and ginsenosides: Therapeutic potential for sarcopenia
Weiwei Zha, Yuanhai Sun, Wenwen Gong, Linghuan Li, Wonnam Kim, Hanbing Li
Biomedicine & Pharmacotherapy.2022; 156: 113876. CrossRef - Bioactive Oligopeptides from Ginseng (Panax ginseng Meyer) Suppress Oxidative Stress-Induced Senescence in Fibroblasts via NAD+/SIRT1/PGC-1α Signaling Pathway
Na Zhu, Mei-Hong Xu, Yong Li
Nutrients.2022; 14(24): 5289. CrossRef - Review of ginsenosides targeting mitochondrial function to treat multiple disorders: Current status and perspectives
Qingxia Huang, Song Gao, Daqing Zhao, Xiangyan Li
Journal of Ginseng Research.2021; 45(3): 371. CrossRef - The Effects of Korean Red Ginseng on Biological Aging and Antioxidant Capacity in Postmenopausal Women: A Double-Blind Randomized Controlled Study
Tae-Ha Chung, Ji-Hye Kim, So-Young Seol, Yon-Ji Kim, Yong-Jae Lee
Nutrients.2021; 13(9): 3090. CrossRef - A comprehensive review on the phytochemistry, pharmacokinetics, and antidiabetic effect of Ginseng
Yage Liu, Hao Zhang, Xuan Dai, Ruyuan Zhu, Beibei Chen, Bingke Xia, Zimengwei Ye, Dandan Zhao, Sihua Gao, Alexander N. Orekhov, Dongwei Zhang, Lili Wang, Shuzhen Guo
Phytomedicine.2021; 92: 153717. CrossRef - Chronic Adipose Tissue Inflammation Linking Obesity to Insulin Resistance and Type 2 Diabetes
Federica Zatterale, Michele Longo, Jamal Naderi, Gregory Alexander Raciti, Antonella Desiderio, Claudia Miele, Francesco Beguinot
Frontiers in Physiology.2020;[Epub] CrossRef - Stereoisomer-specific ginsenoside 20(S)-Rg3 reverses replicative senescence of human diploid fibroblasts via Akt-mTOR-Sirtuin signaling
Kyeong-Eun Yang, Hyun-Jin Jang, In-Hu Hwang, Eun Mi Hong, Min-Goo Lee, Soon Lee, Ik-Soon Jang, Jong-Soon Choi
Journal of Ginseng Research.2020; 44(2): 341. CrossRef - Ginsenosides for the treatment of metabolic syndrome and cardiovascular diseases: Pharmacology and mechanisms
Wenxiang Fan, Yongliang Huang, Hui Zheng, Shuiqin Li, Zhuohong Li, Li Yuan, Xi Cheng, Chengshi He, Jianfeng Sun
Biomedicine & Pharmacotherapy.2020; 132: 110915. CrossRef - Ca2+-activated mitochondrial biogenesis and functions improve stem cell fate in Rg3-treated human mesenchymal stem cells
Taeui Hong, Moon Young Kim, Dat Da Ly, Su Jung Park, Young Woo Eom, Kyu-Sang Park, Soon Koo Baik
Stem Cell Research & Therapy.2020;[Epub] CrossRef - Mitochondrial Dysfunction in Adipocytes as a Primary Cause of Adipose Tissue Inflammation
Chang-Yun Woo, Jung Eun Jang, Seung Eun Lee, Eun Hee Koh, Ki-Up Lee
Diabetes & Metabolism Journal.2019; 43(3): 247. CrossRef - Ginsenoside Rg3 upregulates myotube formation and mitochondrial function, thereby protecting myotube atrophy induced by tumor necrosis factor-alpha
Sang-Jin Lee, Ju Hyun Bae, Hani Lee, Hyunji Lee, Jongsun Park, Jong-Sun Kang, Gyu-Un Bae
Journal of Ethnopharmacology.2019; 242: 112054. CrossRef - Therapeutic Potential of Ginsenosides as an Adjuvant Treatment for Diabetes
Litao Bai, Jialiang Gao, Fan Wei, Jing Zhao, Danwei Wang, Junping Wei
Frontiers in Pharmacology.2018;[Epub] CrossRef - Ginseng and obesity
Zhipeng Li, Geun Eog Ji
Journal of Ginseng Research.2018; 42(1): 1. CrossRef - Molecular signaling of ginsenosides Rb1, Rg1, and Rg3 and their mode of actions
Padmanaban Mohanan, Sathiyamoorthy Subramaniyam, Ramya Mathiyalagan, Deok-Chun Yang
Journal of Ginseng Research.2018; 42(2): 123. CrossRef - Inactivation of glycogen synthase kinase-3β (GSK-3β) enhances skeletal muscle oxidative metabolism
W.F. Theeuwes, H.R. Gosker, R.C.J. Langen, K.J.P. Verhees, N.A.M. Pansters, A.M.W.J. Schols, A.H.V. Remels
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2017; 1863(12): 3075. CrossRef - Anti-Fatigue Effects of Small Molecule Oligopeptides Isolated from Panax ginseng C. A. Meyer in Mice
Lei Bao, Xiaxia Cai, Junbo Wang, Yuan Zhang, Bin Sun, Yong Li
Nutrients.2016; 8(12): 807. CrossRef
- Comparison of Ginseng Leaf Extract and Its Acid-Treated Form, UG0712 Between Their Effects on Exercise Performance in Mice
- Clinical Care/Education
- Hyperglycemia Is Associated with Impaired Muscle Quality in Older Men with Diabetes: The Korean Longitudinal Study on Health and Aging
- Ji Won Yoon, Yong-Chan Ha, Kyoung Min Kim, Jae Hoon Moon, Sung Hee Choi, Soo Lim, Young Joo Park, Jae Young Lim, Ki Woong Kim, Kyong Soo Park, Hak Chul Jang
- Diabetes Metab J. 2016;40(2):140-146. Published online March 31, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.2.140
- 7,302 View
- 78 Download
- 86 Web of Science
- 89 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The study aimed to investigate the influence of hyperglycemia on muscle quality in older men with type 2 diabetes.
Methods This was a subsidiary study of the Korean Longitudinal Study of Health and Aging. Among 326 older men consenting to tests of body composition and muscle strength, 269 men were ultimately analyzed after the exclusion because of stroke (
n =30) and uncertainty about the diagnosis of diabetes (n =27). Body composition was measured using dual-energy X-ray absorptiometry and computed tomography. Muscle strength for knee extension was measured using an isokinetic dynamometer. Muscle quality was assessed from the ratio of leg strength to the entire corresponding leg muscle mass.Results The muscle mass, strength, and quality in patients with type 2 diabetes did not differ significantly from controls. However, when patients with diabetes were subdivided according to their glycemic control status, patients with a glycosylated hemoglobin (HbA1c) level of ≥8.5% showed significantly decreased leg muscle quality by multivariate analysis (odds ratio, 4.510;
P =0.045) after adjustment for age, body mass index, smoking amount, alcohol consumption, physical activity, and duration of diabetes. Physical performance status was also impaired in subjects with an HbA1c of ≥8.5%.Conclusion Poor glycemic control in these older patients with diabetes was associated with significant risk of decreased muscle quality and performance status. Glycemic control with an HbA1c of <8.5% might be needed to reduce the risk of adverse skeletal and functional outcomes in this population.
-
Citations
Citations to this article as recorded by- Downhill running and caloric restriction attenuate insulin resistance associated skeletal muscle atrophy via the promotion of M2-like macrophages through TRIB3-AKT pathway
Wei Luo, Yue Zhou, Qiang Tang, Yuhang Wang, Yansong Liu, Lei Ai
Free Radical Biology and Medicine.2024; 210: 271. CrossRef - Diabetic Sarcopenia. A proposed muscle screening protocol in people with diabetes
Daniel de Luis Román, Juana Carretero Gómez, José Manuel García-Almeida, Fernando Garrachón Vallo, German Guzmán Rolo, Juan José López Gómez, Francisco José Tarazona-Santabalbina, Alejandro Sanz-Paris
Reviews in Endocrine and Metabolic Disorders.2024;[Epub] CrossRef - Dynapenia and sarcopenia: association with the diagnosis, duration and complication of type 2 diabetes mellitus in ELSA-Brasil
Débora Noara Duarte dos Santos, Carolina Gomes Coelho, Maria de Fátima Haueisen Sander Diniz, Bruce Bartholow Duncan, Maria Inês Schmidt, Isabela Judith Martins Bensenor, Claudia Szlejf, Rosa Weiss Telles, Sandhi Maria Barreto
Cadernos de Saúde Pública.2024;[Epub] CrossRef - Breaking Down Cachexia: A Narrative Review on the Prevalence of Cachexia in Cancer Patients and Its Associated Risk Factors
Mahmathi Karuppannan, Fares M. S. Muthanna, Fazlin Mohd Fauzi
Nutrition and Cancer.2024; 76(5): 404. CrossRef - Mechanism of muscle atrophy in a normal-weight rat model of type 2 diabetes established by using a soft-pellet diet
Sayaka Akieda-Asai, Hao Ma, Wanxin Han, Junko Nagata, Fumitake Yamaguchi, Yukari Date
Scientific Reports.2024;[Epub] CrossRef - Morphological and functional changes in skeletal muscle in type 2 diabetes mellitus: A systematic review and meta-analysis
Jardeson Rocha Filgueiras, Cleudiane Pereira Sales, Ivanilson Gomes da Silva, Cristiana Maria Dos Santos, Elias de Carvalho Magalhães Neto, Rebeca Barbosa da Rocha, Vinicius Saura Cardoso
Physiotherapy Theory and Practice.2023; 39(9): 1789. CrossRef - Hypoglycemic drug liraglutide alleviates low muscle mass by inhibiting the expression of MuRF1 and MAFbx in diabetic muscle atrophy
Dongmei Fan, Yue Wang, Bowei Liu, Fuzai Yin
Journal of the Chinese Medical Association.2023; 86(2): 166. CrossRef - Mechanisms underlying altered neuromuscular function in people with DPN
Antonin Le Corre, Nathan Caron, Nicolas A. Turpin, Georges Dalleau
European Journal of Applied Physiology.2023; 123(7): 1433. CrossRef - Effects of body compositions on the associations between ferritin and diabetes parameters among Japanese community dwellers
Kyi Mar Wai, Rei Akuzawa, Yoko Umeda, Wataru Munakata, Yoshiko Takahashi, Shigeyuki Nakaji, Kazushige Ihara
Journal of Trace Elements in Medicine and Biology.2023; 78: 127174. CrossRef - Effects of glycemic control on frailty: a multidimensional perspective
Ahmed H Abdelhafiz
Hospital Practice.2023; 51(3): 124. CrossRef - Hand grip strength is inversely associated with total daily insulin dose requirement in patients with type 2 diabetes mellitus: a cross-sectional study
Da-shuang Chen, Yun-qing Zhu, Wen-ji Ni, Yu-jiao Li, Guo-ping Yin, Zi-yue Shao, Jian Zhu
PeerJ.2023; 11: e15761. CrossRef - Sarcopenia in Type 2 Diabetes Mellitus: Study of the Modifiable Risk Factors Involved
Surapaneni Lakshmi Sravya, Jayshree Swain, Abhay Kumar Sahoo, Swayamsidha Mangaraj, Jayabhanu Kanwar, Pooja Jadhao, Srijit Das
Journal of Clinical Medicine.2023; 12(17): 5499. CrossRef - Salbutamol ameliorates skeletal muscle wasting and inflammatory markers in streptozotocin (STZ)-induced diabetic rats
Anand Kumar, Priyanka Prajapati, Vinit Raj, Seong-Cheol Kim, Vikas Mishra, Chaitany Jayprakash Raorane, Ritu Raj, Dinesh Kumar, Sapana Kushwaha
International Immunopharmacology.2023; 124: 110883. CrossRef - Decreased serum musclin concentration is independently associated with the high prevalence of sarcopenia in Chinese middle‐elderly patients with type 2 diabetes mellitus
Lei Fu, Qing Zhang, Juan Liu, Xiaoqing Yuan, Xinhua Ye
Journal of Diabetes Investigation.2023; 14(12): 1412. CrossRef - Association between relative muscle strength and hypertension in middle-aged and older Chinese adults
Jin-hua Luo, Tu-ming Zhang, Lin-lin Yang, Yu-ying Cai, Yu Yang
BMC Public Health.2023;[Epub] CrossRef - Diabetes Mellitus in the Elderly Adults in Korea: Based on Data from the Korea National Health and Nutrition Examination Survey 2019 to 2020
Seung-Hyun Ko, Kyung Do Han, Yong-Moon Park, Jae-Seung Yun, Kyuho Kim, Jae-Hyun Bae, Hyuk-Sang Kwon, Nan-Hee Kim
Diabetes & Metabolism Journal.2023; 47(5): 643. CrossRef - Management of Hyperglycemia in Older Adults with Type 2 Diabetes
Gunjan Y. Gandhi, Arshag D. Mooradian
Drugs & Aging.2022; 39(1): 39. CrossRef - Deleterious Effect of High-Fat Diet on Skeletal Muscle Performance Is Prevented by High-Protein Intake in Adult Rats but Not in Old Rats
Eleonora Poggiogalle, Fanny Rossignon, Aude Carayon, Fréderic Capel, Jean-Paul Rigaudière, Sarah De Saint Vincent, Olivier Le-Bacquer, Jérôme Salles, Christophe Giraudet, Véronique Patrac, Patrice Lebecque, Stéphane Walrand, Yves Boirie, Vincent Martin, C
Frontiers in Physiology.2022;[Epub] CrossRef - Metabolic phenotypes explain the relationship between dysglycaemia and frailty in older people with type 2 diabetes
A.H. Abdelhafiz, A.J. Sinclair
Journal of Diabetes and its Complications.2022; 36(4): 108144. CrossRef - Altered features of body composition in older adults with type 2 diabetes and prediabetes compared with matched controls
Kirsten E. Bell, Michael T. Paris, Egor Avrutin, Marina Mourtzakis
Journal of Cachexia, Sarcopenia and Muscle.2022; 13(2): 1087. CrossRef - A modern approach to glucose-lowering therapy in frail older people with type 2 diabetes mellitus
Ahmed H. Abdelhafiz, Daniel Pennells, Alan J. Sinclair
Expert Review of Endocrinology & Metabolism.2022; 17(2): 95. CrossRef - Metabolic syndrome and its association with components of sarcopenia in older community-dwelling Chinese
Qiangwei Tong, Xiao Wang, Yunlu Sheng, Shu Chen, Bin Lai, Rong Lv, Jing Yu
The Journal of Biomedical Research.2022; 36(2): 120. CrossRef - Sarcopenia is associated with the Geriatric Nutritional Risk Index in elderly patients with poorly controlled type 2 diabetes mellitus
Shun Matsuura, Koji Shibazaki, Reiko Uchida, Yukiko Imai, Takuya Mukoyama, Shoko Shibata, Hiroshi Morita
Journal of Diabetes Investigation.2022; 13(8): 1366. CrossRef - Increased serum levels of advanced glycation end products are negatively associated with relative muscle strength in patients with type 2 diabetes mellitus
Tsung-Hui Wu, Shiow-Chwen Tsai, Hsuan-Wei Lin, Chiao-Nan Chen, Chii-Min Hwu
BMC Endocrine Disorders.2022;[Epub] CrossRef - Clinical outcomes of multidimensional association of type 2 diabetes mellitus, COVID-19 and sarcopenia: an algorithm and scoping systematic evaluation
Anmar Al-Taie, Oritsetimeyin Arueyingho, Jalal Khoshnaw, Abdul Hafeez
Archives of Physiology and Biochemistry.2022; : 1. CrossRef - Hypoglycaemic therapy in frail older people with type 2 diabetes mellitus—a choice determined by metabolic phenotype
Alan J. Sinclair, Daniel Pennells, Ahmed H. Abdelhafiz
Aging Clinical and Experimental Research.2022; 34(9): 1949. CrossRef - Insulin in Frail, Older People with Type 2 Diabetes—Low Threshold for Therapy
Ahmed Abdelhafiz, Shail Bisht, Iva Kovacevic, Daniel Pennells, Alan Sinclair
Diabetology.2022; 3(2): 369. CrossRef - Sex-Specific Associations Between Low Muscle Mass and Glucose Fluctuations in Patients With Type 2 Diabetes Mellitus
Xiulin Shi, Wenjuan Liu, Lulu Zhang, Fangsen Xiao, Peiying Huang, Bing Yan, Yiping Zhang, Weijuan Su, Qiuhui Jiang, Mingzhu Lin, Wei Liu, Xuejun Li
Frontiers in Endocrinology.2022;[Epub] CrossRef - Lifestyle factors associated with muscle quality in community‐dwelling older people with type 2 diabetes in Japan and Taiwan: a cross‐sectional study
Yuko Yamaguchi, Chieko Greiner, Shu‐Chun Lee, Hirochika Ryuno, Hsin‐Yen Yen, Chiou‐Fen Lin, Ting‐I Lee, Pi‐Hsia Lee
Psychogeriatrics.2022; 22(5): 736. CrossRef - Relationship between Echo Intensity of Vastus Lateralis and Knee Extension Strength in Patients with Type 2 Diabetes Mellitus
Yoshikazu HIRASAWA, Ryosuke MATSUKI, Hideaki TANINA
Physical Therapy Research.2022; 25(3): 113. CrossRef - Time trends (2012–2020) in glycated hemoglobin and adherence to the glycemic targets recommended for elderly patients by the Japan Diabetes Society/Japan Geriatrics Society Joint Committee among memory clinic patients with diabetes mellitus
Taiki Sugimoto, Hisashi Noma, Yujiro Kuroda, Nanae Matsumoto, Kazuaki Uchida, Yoshinobu Kishino, Naoki Saji, Shumpei Niida, Takashi Sakurai
Journal of Diabetes Investigation.2022; 13(12): 2038. CrossRef - Relationship between Diabetes Status and Sarcopenia in Community-Dwelling Older Adults
Kazuhei Nishimoto, Takehiko Doi, Kota Tsutsumimoto, Sho Nakakubo, Satoshi Kurita, Yuto Kiuchi, Hiroyuki Shimada
Journal of the American Medical Directors Association.2022; 23(10): 1718.e7. CrossRef - Low relative hand grip strength is associated with a higher risk for diabetes and impaired fasting glucose among the Korean population
Min Jin Lee, Ah Reum Khang, Dongwon Yi, Yang Ho Kang, Giacomo Pucci
PLOS ONE.2022; 17(10): e0275746. CrossRef - Association between Lower-to-Upper Ratio of Appendicular Skeletal Muscle and Metabolic Syndrome
Hyun Eui Moon, Tae Sic Lee, Tae-Ha Chung
Journal of Clinical Medicine.2022; 11(21): 6309. CrossRef - Association of plasma brain-derived neurotrophic factor levels and frailty in community-dwelling older adults
Eun Roh, Soon Young Hwang, Eyun Song, Min Jeong Park, Hye Jin Yoo, Sei Hyun Baik, Miji Kim, Chang Won Won, Kyung Mook Choi
Scientific Reports.2022;[Epub] CrossRef - Organokines, Sarcopenia, and Metabolic Repercussions: The Vicious Cycle and the Interplay with Exercise
Giulia Minniti, Letícia Maria Pescinini-Salzedas, Guilherme Almeida dos Santos Minniti, Lucas Fornari Laurindo, Sandra Maria Barbalho, Renata Vargas Sinatora, Lance Alan Sloan, Rafael Santos de Argollo Haber, Adriano Cressoni Araújo, Karina Quesada, Jesse
International Journal of Molecular Sciences.2022; 23(21): 13452. CrossRef - Multimorbidity, Frailty and Diabetes in Older People–Identifying Interrelationships and Outcomes
Alan J. Sinclair, Ahmed H. Abdelhafiz
Journal of Personalized Medicine.2022; 12(11): 1911. CrossRef - Determinants of High-Dose Insulin Usage and Upper Extremity Muscle Strength in Adult Patients With Type 2 Diabetes
Eren Imre, Tugce Apaydin, Hatice Gizem Gunhan, Dilek Gogas Yavuz
Canadian Journal of Diabetes.2021; 45(4): 341. CrossRef - Glycemic Control and Insulin Improve Muscle Mass and Gait Speed in Type 2 Diabetes: The MUSCLES-DM Study
Ken Sugimoto, Hiroshi Ikegami, Yasunori Takata, Tomohiro Katsuya, Masahiro Fukuda, Hiroshi Akasaka, Yasuharu Tabara, Haruhiko Osawa, Yoshihisa Hiromine, Hiromi Rakugi
Journal of the American Medical Directors Association.2021; 22(4): 834. CrossRef - A Narrative Review on Sarcopenia in Type 2 Diabetes Mellitus: Prevalence and Associated Factors
Anna Izzo, Elena Massimino, Gabriele Riccardi, Giuseppe Della Pepa
Nutrients.2021; 13(1): 183. CrossRef - Decreased handgrip strength in patients with type 2 diabetes: A cross-sectional study in a tertiary care hospital in north India
Parjeet Kaur, Ritesh Bansal, Bharti Bhargava, Sunil Mishra, Harmandeep Gill, Ambrish Mithal
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2021; 15(1): 325. CrossRef - Factors associated with relative muscle strength in patients with type 2 diabetes mellitus
Chiao-Nan Chen, Ting-Chung Chen, Shiow-Chwen Tsai, Chii-Min Hwu
Archives of Gerontology and Geriatrics.2021; 95: 104384. CrossRef - Newer anti-diabetic therapies with low hypoglycemic risk-potential advantages for frail older people
Demelza Emmerton, Ahmed Abdelhafiz
Hospital Practice.2021; 49(3): 164. CrossRef - Influence of glucose, insulin fluctuation, and glycosylated hemoglobin on the outcome of sarcopenia in patients with type 2 diabetes mellitus
Yuxi Lin, Yongze Zhang, Ximei Shen, Lingning Huang, Sunjie Yan
Journal of Diabetes and its Complications.2021; 35(6): 107926. CrossRef - Presence and Implications of Sarcopenia in Non-alcoholic Steatohepatitis
Gregory Habig, Christa Smaltz, Dina Halegoua-DeMarzio
Metabolites.2021; 11(4): 242. CrossRef - Sensory-Motor Mechanisms Increasing Falls Risk in Diabetic Peripheral Neuropathy
Neil D. Reeves, Giorgio Orlando, Steven J. Brown
Medicina.2021; 57(5): 457. CrossRef - Impact of frailty metabolic phenotypes on the management of older people with type 2 diabetes mellitus
Ahmed H Abdelhafiz, Demelza Emmerton, Alan J Sinclair
Geriatrics & Gerontology International.2021; 21(8): 614. CrossRef - Type 2 diabetes mellitus in older adults: clinical considerations and management
Srikanth Bellary, Ioannis Kyrou, James E. Brown, Clifford J. Bailey
Nature Reviews Endocrinology.2021; 17(9): 534. CrossRef - Metabolic Syndrome and Sarcopenia
Hiroki Nishikawa, Akira Asai, Shinya Fukunishi, Shuhei Nishiguchi, Kazuhide Higuchi
Nutrients.2021; 13(10): 3519. CrossRef - Angiotensin II inhibition: a potential treatment to slow the progression of sarcopenia
Jeffrey Kingsley, Keiichi Torimoto, Tomoki Hashimoto, Satoru Eguchi
Clinical Science.2021; 135(21): 2503. CrossRef - Muscle strength, an independent determinant of glycemic control in older adults with long-standing type 2 diabetes: a prospective cohort study
Bo Kyung Koo, Seoil Moon, Min Kyong Moon
BMC Geriatrics.2021;[Epub] CrossRef - Associations between homocysteine, inflammatory cytokines and sarcopenia in Chinese older adults with type 2 diabetes
Zhi-Jing Mu, Jun-Ling Fu, Li-Na Sun, Piu Chan, Shuang-Ling Xiu
BMC Geriatrics.2021;[Epub] CrossRef - The Association Between Diabetes Mellitus and Risk of Sarcopenia: Accumulated Evidences From Observational Studies
Yu-Shun Qiao, Yin-He Chai, Hong-Jian Gong, Zhiyessova Zhuldyz, Coen D. A. Stehouwer, Jian-Bo Zhou, Rafael Simó
Frontiers in Endocrinology.2021;[Epub] CrossRef - The utility of the ultrasonographic assessment of the lower leg muscles to evaluate sarcopenia and muscle quality in older adults
Masaaki Isaka, Ken Sugimoto, Taku Fujimoto, Yukiko Yasunobe, Keyu Xie, Yuri Onishi, Shino Yoshida, Toshimasa Takahashi, Hitomi Kurinami, Hiroshi Akasaka, Yasushi Takeya, Koichi Yamamoto, Hiromi Rakugi
JCSM Clinical Reports.2021; 6(2): 53. CrossRef - Associations between grip strength and glycemic control in type 2 diabetes mellitus: an analysis of data from the 2014-2019 Korea National Health and Nutrition Examination Survey
Harim Choe, Hoyong Sung, Geon Hui Kim, On Lee, Hyo Youl Moon, Yeon Soo Kim
Epidemiology and Health.2021; 43: e2021080. CrossRef - Uncontrolled Diabetes as an Associated Factor with Dynapenia in Adults Aged 50 Years or Older: Sex Differences
Clarice Cavalero Nebuloni, Roberta de Oliveira Máximo, Cesar de Oliveira, Tiago da Silva Alexandre, Anne Newman
The Journals of Gerontology: Series A.2020; 75(6): 1191. CrossRef - Identification and prevalence of frailty in diabetes mellitus and association with clinical outcomes: a systematic review protocol
Peter Hanlon, Isabella Fauré, Neave Corcoran, Elaine Butterly, Jim Lewsey, David A McAllister, Frances S Mair
BMJ Open.2020; 10(9): e037476. CrossRef - Longitudinal association of type 2 diabetes and insulin therapy with muscle parameters in the KORA-Age study
Uta Ferrari, Cornelia Then, Marietta Rottenkolber, Canan Selte, Jochen Seissler, Romy Conzade, Birgit Linkohr, Annette Peters, Michael Drey, Barbara Thorand
Acta Diabetologica.2020; 57(9): 1057. CrossRef - Triad of impairment in older people with diabetes-reciprocal relations and clinical implications
A.H. Abdelhafiz, P.C. Davies, A.J. Sinclair
Diabetes Research and Clinical Practice.2020; 161: 108065. CrossRef - Physical activity and exercise: Strategies to manage frailty
Javier Angulo, Mariam El Assar, Alejandro Álvarez-Bustos, Leocadio Rodríguez-Mañas
Redox Biology.2020; 35: 101513. CrossRef - Handgrip measurement as a useful benchmark for locomotive syndrome in patients with type 2 diabetes mellitus: A KAMOGAWA‐DM cohort study
Noriyuki Kitagawa, Takuro Okamura, Nobuko Kitagawa, Yoshitaka Hashimoto, Masahide Hamaguchi, Michiaki Fukui
Journal of Diabetes Investigation.2020; 11(6): 1602. CrossRef - Edmonton frail score is associated with diabetic control in elderly type 2 diabetic subjects
Satilmis Bilgin, Gulali Aktas, Ozge Kurtkulagi, Burcin M. Atak, Tuba T. Duman
Journal of Diabetes & Metabolic Disorders.2020; 19(1): 511. CrossRef - Comparison of field- and laboratory-based estimates of muscle quality index between octogenarians and young older adults: an observational study
Dahan da Cunha Nascimento, Jonato Prestes, Joyce de Sousa Diniz, Pedro Rodrigues Beal, Vicente Paulo Alves, Whitley Stone, Fabiani Lage Rodrigues Beal
Journal of Exercise Rehabilitation.2020; 16(5): 458. CrossRef - Tip 2 Diyabetli Hastalarda Kan Glukoz Seviyesi ile Kas Gücü, Propriosepsiyon ve Vücut Kompozisyonu Arasındaki İlişki
Zahide Betül TAYFUR, Esra ATILGAN
Turkish Journal of Diabetes and Obesity.2020; 4(3): 207. CrossRef - Challenges and Strategies for Diabetes Management in Community-Living Older Adults
Alan J. Sinclair, Ahmed H. Abdelhafiz
Diabetes Spectrum.2020; 33(3): 217. CrossRef - Association between deterioration in muscle strength and peripheral neuropathy in people with diabetes
Tae Jung Oh, Sunyoung Kang, Jie-Eun Lee, Jae Hoon Moon, Sung Hee Choi, Soo Lim, Hak Chul Jang
Journal of Diabetes and its Complications.2019; 33(8): 598. CrossRef - The Association between Body Composition using Dual energy X-ray Absorptiometry and Type-2 Diabetes: A Systematic Review and Meta-Analysis of Observational studies
Preeti Gupta, Carla Lanca, Alfred T. L. Gan, Pauline Soh, Sahil Thakur, Yijin Tao, Neelam Kumari, Ryan E. K. Man, Eva K. Fenwick, Ecosse L. Lamoureux
Scientific Reports.2019;[Epub] CrossRef - MECHANISMS OF ENDOCRINE DISEASE: Sarcopenia in endocrine and non-endocrine disorders
Victoria Zeghbi Cochenski Borba, Tatiana Lemos Costa, Carolina Aguiar Moreira, Cesar Luiz Boguszewski
European Journal of Endocrinology.2019; 180(5): R185. CrossRef - Hyperglycemia induces skeletal muscle atrophy via a WWP1/KLF15 axis
Yu Hirata, Kazuhiro Nomura, Yoko Senga, Yuko Okada, Kenta Kobayashi, Shiki Okamoto, Yasuhiko Minokoshi, Michihiro Imamura, Shin’ichi Takeda, Tetsuya Hosooka, Wataru Ogawa
JCI Insight.2019;[Epub] CrossRef - Hyperglycemia in non‐obese patients with type 2 diabetes is associated with low muscle mass: The Multicenter Study for Clarifying Evidence for Sarcopenia in Patients with Diabetes Mellitus
Ken Sugimoto, Yasuharu Tabara, Hiroshi Ikegami, Yasunori Takata, Kei Kamide, Tome Ikezoe, Eri Kiyoshige, Yukako Makutani, Hiroshi Onuma, Yasuyuki Gondo, Kazunori Ikebe, Noriaki Ichihashi, Tadao Tsuboyama, Fumihiko Matsuda, Katsuhiko Kohara, Mai Kabayama,
Journal of Diabetes Investigation.2019; 10(6): 1471. CrossRef - Diabetic Peripheral Neuropathy as a Risk Factor for Sarcopenia
Tae Jung Oh, Yoojung Song, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
Annals of Geriatric Medicine and Research.2019; 23(4): 170. CrossRef - Diabetes and frailty
Mariam El Assar, Olga Laosa, Leocadio Rodríguez Mañas
Current Opinion in Clinical Nutrition & Metabolic Care.2019; 22(1): 52. CrossRef - Association of Glucose Fluctuations with Sarcopenia in Older Adults with Type 2 Diabetes Mellitus
Noriko Ogama, Takashi Sakurai, Shuji Kawashima, Takahisa Tanikawa, Haruhiko Tokuda, Shosuke Satake, Hisayuki Miura, Atsuya Shimizu, Manabu Kokubo, Shumpei Niida, Kenji Toba, Hiroyuki Umegaki, Masafumi Kuzuya
Journal of Clinical Medicine.2019; 8(3): 319. CrossRef - Diabetes in the elderly
Ahmed H. Abdelhafiz, Alan J. Sinclair
Medicine.2019; 47(2): 119. CrossRef - Diabetes and Muscle Dysfunction in Older Adults
Hak Chul Jang
Annals of Geriatric Medicine and Research.2019; 23(4): 160. CrossRef - Factors influencing safe glucose-lowering in older adults with type 2 diabetes: A PeRsOn-centred ApproaCh To IndiVidualisEd (PROACTIVE) Glycemic Goals for older people
C.E. Hambling, K. Khunti, X. Cos, J. Wens, L. Martinez, P. Topsever, S. Del Prato, A. Sinclair, G. Schernthaner, G. Rutten, S. Seidu
Primary Care Diabetes.2019; 13(4): 330. CrossRef - Effects of resistance training on neuromuscular parameters in elderly with type 2 diabetes mellitus: A randomized clinical trial
Cíntia E. Botton, Daniel Umpierre, Anderson Rech, Lucinéia O. Pfeifer, Carlos L.F. Machado, Juliana L. Teodoro, Alexandre S. Dias, Ronei S. Pinto
Experimental Gerontology.2018; 113: 141. CrossRef - Management of Elderly Diabetes Patients Who Are Unable to Self-Care
Bok Rye Song
The Journal of Korean Diabetes.2018; 19(4): 232. CrossRef - Decreased Muscle Strength and Quality in Diabetes-Related Dementia
Akito Tsugawa, Yusuke Ogawa, Naoto Takenoshita, Yoshitsugu Kaneko, Hirokuni Hatanaka, Eriko Jaime, Raita Fukasawa, Haruo Hanyu
Dementia and Geriatric Cognitive Disorders Extra.2017; 7(3): 454. CrossRef - Diabetes and Sarcopenia
Dong Hyun Kim, Tae Yang Yu
The Journal of Korean Diabetes.2017; 18(4): 239. CrossRef - Frailty and sarcopenia - newly emerging and high impact complications of diabetes
Alan J. Sinclair, Ahmed H. Abdelhafiz, Leocadio Rodríguez-Mañas
Journal of Diabetes and its Complications.2017; 31(9): 1465. CrossRef - Association of diabetic retinopathy with both sarcopenia and muscle quality in patients with type 2 diabetes: a cross-sectional study
Tatsuya Fukuda, Ryotaro Bouchi, Takato Takeuchi, Yujiro Nakano, Masanori Murakami, Isao Minami, Hajime Izumiyama, Koshi Hashimoto, Takanobu Yoshimoto, Yoshihiro Ogawa
BMJ Open Diabetes Research & Care.2017; 5(1): e000404. CrossRef - Practical considerations for managing patients with diabetes and dementia
Michelle L Mair, Rohin Athavale, Ahmed H Abdelhafiz
Expert Review of Endocrinology & Metabolism.2017; 12(6): 429. CrossRef - Sarcopenia: An Endocrine Disorder?
Alexis McKee, John E. Morley, Alvin M. Matsumoto, Aaron Vinik
Endocrine Practice.2017; 23(9): 1143. CrossRef - Response: Hyperglycemia Is Associated with Impaired Muscle Quality in Older Men with Diabetes: The Korean Longitudinal Study on Health and Aging (Diabetes Metab J 2016;40:140-6)
Ji Won Yoon, Hak Chul Jang
Diabetes & Metabolism Journal.2016; 40(3): 250. CrossRef - Salivary lactate dehydrogenase and aminotransferases in diabetic patients
Barbara Malicka, Katarzyna Skoskiewicz-Malinowska, Urszula Kaczmarek
Medicine.2016; 95(47): e5211. CrossRef - Explanatory models of muscle performance in acromegaly patients evaluated by knee isokinetic dynamometry: Implications for rehabilitation
Agnaldo José Lopes, Arthur Sá Ferreira, Evelyn Mendes Walchan, Mauricio Santos Soares, Priscila Santos Bunn, Fernando Silva Guimarães
Human Movement Science.2016; 49: 160. CrossRef - Letter: Hyperglycemia Is Associated with Impaired Muscle Quality in Older Men with Diabetes: The Korean Longitudinal Study on Health and Aging (Diabetes Metab J 2016;40:140-6)
Jun Sung Moon
Diabetes & Metabolism Journal.2016; 40(3): 248. CrossRef - Sarcopenia, Frailty, and Diabetes in Older Adults
Hak Chul Jang
Diabetes & Metabolism Journal.2016; 40(3): 182. CrossRef
- Downhill running and caloric restriction attenuate insulin resistance associated skeletal muscle atrophy via the promotion of M2-like macrophages through TRIB3-AKT pathway
- Clinical Care/Education
- Clinical Characteristics and Metabolic Predictors of Rapid Responders to Dipeptidyl Peptidase-4 Inhibitor as an Add-on Therapy to Sulfonylurea and Metformin
- Ye An Kim, Won Sang Yoo, Eun Shil Hong, Eu Jeong Ku, Kyeong Seon Park, Soo Lim, Young Min Cho, Kyong Soo Park, Hak Chul Jang, Sung Hee Choi
- Diabetes Metab J. 2015;39(6):489-497. Published online November 27, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.6.489
- 3,502 View
- 39 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Dipeptidyl peptidase-4 (DPP-4) inhibitor add-on therapy is a new option for patients with inadequately controlled type 2 diabetes who are taking combined metformin and sulfonylurea (SU). We evaluated the efficacy and safety of this triple therapy and the characteristics of rapid responders and hypoglycemia-prone patients.
Methods We included 807 patients with type 2 diabetes who were prescribed a newly added DPP-4 inhibitor to ongoing metformin and SU in 2009 to 2011. Glycemia and other metabolic parameters at baseline, 12, 24, and 52 weeks, as well as episodes of hypoglycemia were analyzed. Rapid responders were defined as patients with ≥25% reduction in glycosylated hemoglobin (HbA1c) within 12 weeks.
Results At baseline, while on the submaximal metformin and SU combination, the mean HbA1c level was 8.4%. Twelve weeks after initiation of DPP-4 inhibitor add-on, 269 patients (34.4%) achieved an HbA1c level ≤7%. Sixty-six patients (8.2%, 47 men) were rapid responders. The duration of diabetes was shorter in rapid responders, and their baseline fasting plasma glucose (FPG), HbA1c, C-peptide, and homeostasis model assessment of insulin resistance were significantly higher. Patients who experienced hypoglycemia after taking DPP-4 inhibitor add-on were more likely to be female, to have a lower body weight and lower triglyceride and FPG levels, and to have higher homeostasis model assessment of β-cells.
Conclusion An oral hypoglycemic triple agent combination including a DPP-4 inhibitor was effective in patients with uncontrolled diabetes. Proactive dose reduction of SU should be considered when a DPP-4 inhibitor is added for rapid responders and hypoglycemia-prone patients.
-
Citations
Citations to this article as recorded by- A genetic variant in GLP1R is associated with response to DPP-4 inhibitors in patients with type 2 diabetes
Eugene Han, Hye Sun Park, Obin Kwon, Eun Yeong Choe, Hye Jin Wang, Yong-ho Lee, Sang-Hak Lee, Chul Hoon Kim, Lee-Kyung Kim, Soo Heon Kwak, Kyong Soo Park, Chul Sik Kim, Eun Seok Kang
Medicine.2016; 95(44): e5155. CrossRef
- A genetic variant in GLP1R is associated with response to DPP-4 inhibitors in patients with type 2 diabetes
- Optimal Waist Circumference Cutoff Value Based on Insulin Resistance and Visceral Obesity in Koreans with Type 2 Diabetes
- Jung Soo Lim, Young Ju Choi, Soo-Kyung Kim, Byoung Wook Huh, Eun Jig Lee, Kap Bum Huh
- Diabetes Metab J. 2015;39(3):253-263. Published online April 24, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.3.253
- 4,277 View
- 28 Download
- 10 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Visceral obesity is the most powerful contributor to the development of metabolic syndrome (MetS) and cardiovascular diseases. In light of visceral obesity, however, there is a paucity of data on the appropriate cutoff point of waist circumference (WC) in subjects with type 2 diabetes. The aim of this study was to investigate the optimal cutoff value for WC that signals insulin resistance (IR) and visceral obesity in Koreans with type 2 diabetes.
Methods We evaluated 4,252 patients with type 2 diabetes (male 2,220, female 2,032, mean age 57.24 years) who visited our clinic between January 2003 and June 2009. WC was measured at the midpoint between the lower rib and the iliac crest, and insulin sensitivity was assessed by the rate constant of plasma glucose disappearance (
Kitt %/min) using an insulin tolerance test. Visceral fat thickness was measured using ultrasonography. Statistical analysis was performed using receiver operating characteristic curve.Results The optimal cutoff points for WC for identifying the presence of IR and visceral obesity, as well as two or more metabolic components, were 87 cm for men and 81 cm for women. Moreover, these cutoff points had the highest predictive powers for the presence of visceral obesity. The MetS defined by new criteria correlated with the increased carotid intima-media thickness in female subjects.
Conclusion Our results suggest that the optimal cutoff values for WC in Koreans with type 2 diabetes should be reestablished based on IR and visceral obesity.
-
Citations
Citations to this article as recorded by- Association between Muscle Mass, Body Fat Mass, and Abdominal Circumstances with Insulin Resistance among Young Adult Population with Prediabetes Risk
Anindya Putri Adhisti, Siti Fatimah-Muis, Amalia Sukmadianti, Darmono S.S., Febe Christianto
The Indian Journal of Nutrition and Dietetics.2023; : 176. CrossRef - Brazil nut prevents oxidative DNA damage in type 2 diabetes patients
Tamires Pavei Macan, Thais Aquino de Amorim, Adriani Paganini Damiani, Ângela Caroline da Luz Beretta, Marina Lummertz Magenis, Thais Ceresér Vilela, João Paulo Teixeira, Vanessa Moraes de Andrade
Drug and Chemical Toxicology.2022; 45(3): 1066. CrossRef - Metabolic Syndrome and Breast Cancer Molecular Subtypes: An Observational Patient Study
Dafina Ademi-Islami, Suzana Manxhuka-Kerliu, Dhurata Tarifa-Koroveshi, Rozafa Koliqi, Blerim Mujaj
Breast Cancer: Basic and Clinical Research.2022; 16: 117822342210805. CrossRef - Performance of Two Novel Obesity Indicators for the Management of Metabolic Syndrome in Young Adults
Xiaoli Liu, Chunpeng Ma, Fuzai Yin, Rui Wang, Qiang Lu, Na Lu, Chunming Ma
Frontiers in Endocrinology.2021;[Epub] CrossRef - Differential effect of subcutaneous abdominal and visceral adipose tissue on cardiometabolic risk
Susan Sam
Hormone Molecular Biology and Clinical Investigation.2018;[Epub] CrossRef - Three novel obese indicators perform better in monitoring management of metabolic syndrome in type 2 diabetes
Chun-Ming Ma, Na Lu, Rui Wang, Xiao-Li Liu, Qiang Lu, Fu-Zai Yin
Scientific Reports.2017;[Epub] CrossRef - Association between Body Weight Changes and Menstrual Irregularity: The Korea National Health and Nutrition Examination Survey 2010 to 2012
Kyung Min Ko, Kyungdo Han, Youn Jee Chung, Kun-Ho Yoon, Yong Gyu Park, Seung-Hwan Lee
Endocrinology and Metabolism.2017; 32(2): 248. CrossRef - The renal tubular damage marker urinary N-acetyl-β-d-glucosaminidase may be more closely associated with early detection of atherosclerosis than the glomerular damage marker albuminuria in patients with type 2 diabetes
So Ra Kim, Yong-ho Lee, Sang-Guk Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Cardiovascular Diabetology.2017;[Epub] CrossRef - The association between metabolic health, obesity phenotype and the risk of breast cancer
Yong‐Moon Mark Park, Alexandra J. White, Hazel B. Nichols, Katie M. O'Brien, Clarice R. Weinberg, Dale P. Sandler
International Journal of Cancer.2017; 140(12): 2657. CrossRef - Reappraisal of waist circumference cutoff value according to general obesity
Kyung-Soo Kim, Hyun-Ju Oh, Young Ju Choi, Byung Wook Huh, Soo-Kyung Kim, Seok Won Park, Eun Jig Lee, Yong-Wook Cho, Kap-Bum Huh
Nutrition & Metabolism.2016;[Epub] CrossRef
- Association between Muscle Mass, Body Fat Mass, and Abdominal Circumstances with Insulin Resistance among Young Adult Population with Prediabetes Risk
- Therapeutic Approaches for Preserving or Restoring Pancreatic β-Cell Function and Mass
- Kyong Yeun Jung, Kyoung Min Kim, Soo Lim
- Diabetes Metab J. 2014;38(6):426-436. Published online December 15, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.6.426
- 6,118 View
- 115 Download
- 20 Web of Science
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader The goal for the treatment of patients with diabetes has today shifted from merely reducing glucose concentrations to preventing the natural decline in β-cell function and delay the progression of disease. Pancreatic β-cell dysfunction and decreased β-cell mass are crucial in the development of diabetes. The β-cell defects are the main pathogenesis in patients with type 1 diabetes and are associated with type 2 diabetes as the disease progresses. Recent studies suggest that human pancreatic β-cells have a capacity for increased proliferation according to increased demands for insulin. In humans, β-cell mass has been shown to increase in patients showing insulin-resistance states such as obesity or in pregnancy. This capacity might be useful for identifying new therapeutic strategies to reestablish a functional β-cell mass. In this context, therapeutic approaches designed to increase β-cell mass might prove a significant way to manage diabetes and prevent its progression. This review describes the various β-cell defects that appear in patients with diabetes and outline the mechanisms of β-cell failure. We also review common methods for assessing β-cell function and mass and methodological limitations
in vivo . Finally, we discuss the current therapeutic approaches to improve β-cell function and increase β-cell mass.-
Citations
Citations to this article as recorded by- Polychlorinated biphenyls exposure and type 2 diabetes: Molecular mechanism that causes insulin resistance and islet damage
Qiuli Shan, Jingyu Liu, Fan Qu, Anhui Chen, Wenxing He
Environmental Toxicology.2024; 39(4): 2466. CrossRef - Beta‐cell function in type 2 diabetes (T2DM): Can it be preserved or enhanced?
Laure Sayyed Kassem, Aman Rajpal, Margarita Victoria Barreiro, Faramarz Ismail‐Beigi
Journal of Diabetes.2023; 15(10): 817. CrossRef - Preliminary Evaluation of Potential Properties of Three Probiotics and Their Combination with Prebiotics on GLP-1 Secretion and Type 2 Diabetes Alleviation
Ran Xiao, Ran Wang, Shusen Li, Xiaohong Kang, Yimei Ren, Erna Sun, Chenyuan Wang, Jingjing He, Jing Zhan, Wen Yi Kang
Journal of Food Quality.2022; 2022: 1. CrossRef - Preservation effect of imeglimin on pancreatic β-cell mass: Noninvasive evaluation using 111In-exendin-4 SPECT/CT imaging and the perspective of mitochondrial involvements
Muhammad Fauzi, Takaaki Murakami, Hiroyuki Fujimoto, Ainur Botagarova, Kentaro Sakaki, Sakura Kiyobayashi, Masahito Ogura, Nobuya Inagaki
Frontiers in Endocrinology.2022;[Epub] CrossRef - Effects of boschnaloside from Boschniakia rossica on dysglycemia and islet dysfunction in severely diabetic mice through modulating the action of glucagon-like peptide-1
Lie-Chwen Lin, Lin-Chien Lee, Cheng Huang, Chiung-Tong Chen, Jen-Shin Song, Young-Ji Shiao, Hui-Kang Liu
Phytomedicine.2019; 62: 152946. CrossRef - The Potential of Hibiscus sabdariffa Linn in Inducing Glucagon-Like Peptide-1 via SGLT-1 and GLPR in DM Rats
Neng Tine Kartinah, Fadilah Fadilah, Ermita Ilyas Ibrahim, Yuliana Suryati
BioMed Research International.2019; 2019: 1. CrossRef - Efficacy of short‑term intensive treatment with insulin pump to improve islet β‑cell function in newly diagnosed type 2 diabetes via inhibition of oxidative stress
Hai‑Tong Liu, Yan Gao
Experimental and Therapeutic Medicine.2019;[Epub] CrossRef - When metformin is not enough: Pros and cons of SGLT2 and DPP‐4 inhibitors as a second line therapy
Angelo Avogaro, Elías Delgado, Ildiko Lingvay
Diabetes/Metabolism Research and Reviews.2018;[Epub] CrossRef - Metformin prevents glucotoxicity by alleviating oxidative and ER stress–induced CD36 expression in pancreatic beta cells
Jun Sung Moon, Udayakumar Karunakaran, Suma Elumalai, In-Kyu Lee, Hyoung Woo Lee, Yong-Woon Kim, Kyu Chang Won
Journal of Diabetes and its Complications.2017; 31(1): 21. CrossRef - The variability in beta‐cell function in placebo‐treated subjects with type 2 diabetes: application of the weight‐HbA1c‐insulin‐glucose (WHIG) model
Janna K. Duong, Willem de Winter, Steve Choy, Nele Plock, Himanshu Naik, Walter Krauwinkel, Sandra A.G. Visser, Katia M. Verhamme, Miriam C. Sturkenboom, B.H. Stricker, Meindert Danhof
British Journal of Clinical Pharmacology.2017; 83(3): 487. CrossRef - Regulation of pancreatic β-cell function and mass dynamics by prostaglandin signaling
Bethany A. Carboneau, Richard M. Breyer, Maureen Gannon
Journal of Cell Communication and Signaling.2017; 11(2): 105. CrossRef - Effects of low intensity laser acupoint irradiation on inhibiting islet beta-cell apoptosis in rats with type 2 diabetes
Guoxin Xiong, Leilei Xiong, Xinzhong Li
Laser Physics.2016; 26(9): 095605. CrossRef - Effects of continuous positive airway pressure treatment on glucose metabolism in patients with obstructive sleep apnea
Elisabet Martínez-Ceron, Isabel Fernández-Navarro, Francisco Garcia-Rio
Sleep Medicine Reviews.2016; 25: 121. CrossRef - Efficacy and safety of teneligliptin, a novel dipeptidyl peptidase‐4 inhibitor, in Korean patients with type 2 diabetes mellitus: a 24‐week multicentre, randomized, double‐blind, placebo‐controlled phase III trial
S. Hong, C.‐Y. Park, K. A. Han, C. H. Chung, B. J. Ku, H. C. Jang, C. W. Ahn, M.‐K. Lee, M. K. Moon, H. S. Son, C. B. Lee, Y.‐W. Cho, S.‐W. Park
Diabetes, Obesity and Metabolism.2016; 18(5): 528. CrossRef - Senp2 expression was induced by chronic glucose stimulation in INS1 cells, and it was required for the associated induction of Ccnd1 and Mafa
Hye Seung Jung, Yu Mi Kang, Ho Seon Park, Byung Yong Ahn, Hakmo Lee, Min Joo Kim, Jin Young Jang, Sun-Whe Kim
Islets.2016; 8(6): 207. CrossRef - ANTIDIABETIC EVALUATION OF CHONEMORPHA MACROPHYLLA ROOTS BY IN VIVO METHODS USING MALE WISTAR ALBINO RATS AND ITS MECHANISM OF ACTION
K. R. Krishna Kumar, K. K. Srinivasan
INDIAN DRUGS.2016; 53(12): 42. CrossRef - Comparative gene expression profiles in pancreatic islets associated with agouti yellow mutation and PACAP overexpression in mice
Kazuya Ikeda, Shuhei Tomimoto, Soken Tsuchiya, Ken-ichi Hamagami, Norihito Shintani, Yukihiko Sugimoto, Atsushi Ichikawa, Atsushi Kasai, Takanobu Nakazawa, Kazuki Nagayasu, Atsuko Hayata-Takano, Akemichi Baba, Hitoshi Hashimoto
Biochemistry and Biophysics Reports.2015; 2: 179. CrossRef - Therapeutic efficacy of umbilical cord-derived mesenchymal stem cells in patients with type 2 diabetes
LI-XUE GUAN, HUI GUAN, HAI-BO LI, CUI-AI REN, LIN LIU, JIN-JIN CHU, LONG-JUN DAI
Experimental and Therapeutic Medicine.2015; 9(5): 1623. CrossRef - p13 overexpression in pancreatic β-cells ameliorates type 2 diabetes in high-fat-fed mice
Shintaro Higashi, Kazuhiko Katagi, Norihito Shintani, Kazuya Ikeda, Yukihiko Sugimoto, Soken Tsuchiya, Naoki Inoue, Shota Tanaka, Mai Koumoto, Atsushi Kasai, Takanobu Nakazawa, Atsuko Hayata-Takano, Ken-Ichi Hamagami, Shuhei Tomimoto, Takuya Yoshida, Tada
Biochemical and Biophysical Research Communications.2015; 461(4): 612. CrossRef
- Polychlorinated biphenyls exposure and type 2 diabetes: Molecular mechanism that causes insulin resistance and islet damage

 KDA
KDA
 First
First Prev
Prev





